A new review discusses how neutrophils release toxic substances into the body under inflammatory conditions, detailing one of the ways in which chronic inflammation causes long-term damage.
Casting a deadly NET
As we age, we suffer from the ever-increasing chronic inflammation known as inflammaging. This persistent, smoldering background of low-grade inflammation harms wound healing and promotes multiple age-related diseases. Senescent cells, a weakened immune system, and chronic infections are all proposed to contribute to inflammaging.
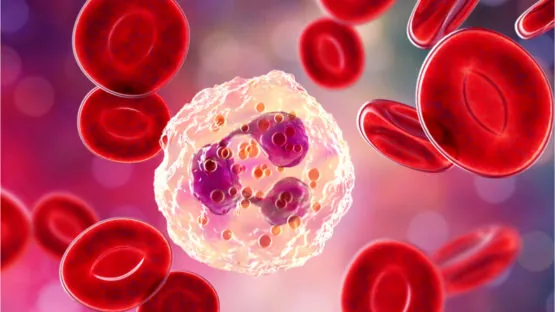
This review focuses on neutrophils, which are immune cells that make up between 55-70 percent of our total white blood cells. Neutrophils are produced in the bone marrow and help prevent infections by inhibiting, crippling, and consuming invading pathogens and foreign particles. They also communicate with other types of cells to help them repair damage and mount a proper immune response.
When they detect inflammation, neutrophils engage in multiple forms of defense, and one of these mechanisms is the formation of neutrophil extracellular traps (NETs) to catch and kill invading bacteria; they do this either while still alive or through NETosis, which is a form of self-sacrifice [1]. Under the circumstances for which they evolved, this is beneficial; the NET catches the invader, the inflammation dies down, and the body heals from the infection.
However, in an environment of chronic inflammation, these cells extrude NETs for no good purpose, and the buildup of these traps potentially leads to lung fibrosis, arthritis, autoimmune disorders, and other conditions [2].
AbstractNeutrophils are an absolutely essential part of the innate immune system, playing an essential role in the control of infectious diseases but more recently are also being viewed as important players in tissue repair. Neutrophils are able to counteract an infection through phagocytosis and/or the release of neutrophil extracellular traps (NETs). By contrast, neutrophils help repair damaged tissues limiting NET production but still phagocytosing debris. However, when inflammation is recurrent, or the inciting agent persists, neutrophils through a frustrated inability to resolve the problem can release NETs to exacerbate tissue damage during inappropriate inflammation. In this review, we will discuss the mechanisms of NET formation, as well as the apparent paradoxical role of neutrophils and NETs in host defense, chronic inflammation and tissue disrepair.
Conclusion
As the immune system declines and becomes more dysfunctional with age, immune responses are inappropriately activated, thus contributing to chronic inflammation. As this review shows, excessive NET formation is one of the ways in which this chronic inflammation leads to long-term damage.
Therapies that reduce chronic inflammation may be able to deal with this problem, and there are several approaches currently in development. The effective management of inflammaging has the potential to promote tissue repair and regeneration while ameliorating various age-related diseases.
Literature
[1] Kaplan, M. J., & Radic, M. (2012). Neutrophil extracellular traps: double-edged swords of innate immunity. The Journal of Immunology, 189(6), 2689-2695.
[2] Castanheira, F. V., & Kubes, P. (2019). Neutrophils and NETS in modulating acute and chronic inflammation. Blood, (), blood-2018-11-844530. Accessed March 24, 2019. https://doi.org/10.1182/blood-2018-11-844530.