Chondroitin Sulfate: Benefits, Side Effects, and Research
Chondroitin sulfate, widely known as chondroitin, has been shown to reduce mortality by a whopping 39% in a cohort of U.S. adults when taken with glucosamine [1]. For an equivalent mortality reduction from moderate exercise, the average person would have to walk one marathon per week [2].
What is chondroitin sulfate?
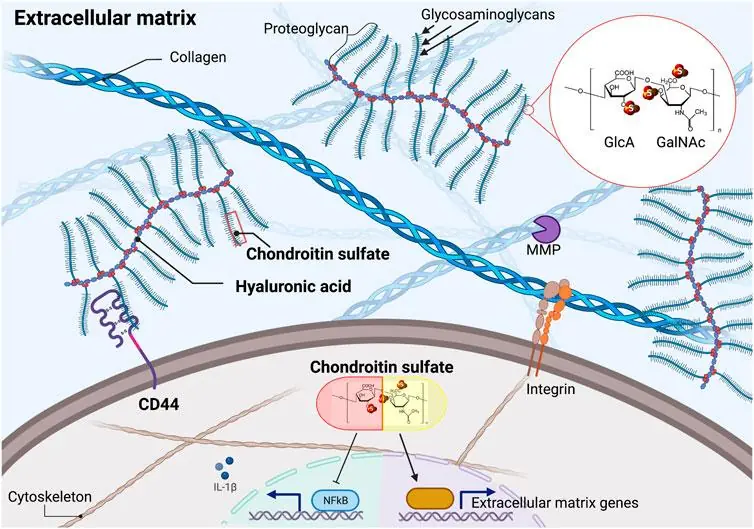
Chondroitin is a key component of cartilage and an essential building block in a very large family of glycated proteins known as glycosaminoglycans (GAGs). These compounds play a wide range of roles, including cell adhesion, proliferation and migration, ECM assembly, tissue repair, coagulation, and immune responses [3]. The modest effects on cartilage and joint inflammation are a minor part of the true value of this endogenous compound.
Its core protein looks like a bottle brush and functions like a shock absorber [4]. antioxidant, anti-apoptosis agent, anti-inflammatory, antimicrobial, anticoagulant, and component in a diverse array of signaling molecules that regulate just about everything [3,5,6].
Chondroitin protects cells from mechanical damage. The bristle-like portions of this molecule carry a negative charge, which attracts and holds water molecules [4]. The combination of water and chondroitin forms a gel with remarkable shock absorption properties [7].
Protection in multiple ways
When linear force is applied to tissues containing chondroitin, it is like punching a water-filled sponge. The force is absorbed and split in every direction as water is displaced from the point of impact. This prevents cells from being damaged. Your body without this engineering feature would be like a car without shocks.
Chondroitin-4-sulfate is one of several chondroitin variants. It inhibits the oxidative damage that hydrogen peroxide causes to fats, which is one of the main sources of free radical damage [5].
Apoptosis, also known as programmed cell death, is often triggered by oxidative damage. Chondroitin-4-sulfate is particularly adept at preventing oxidative burst, the rapid transient burst of reactive oxygen species released from immune cells. Oxidative burst often activates compounds called caspases, which initiate apoptosis [5]. This phenomenon is very pronounced in osteoarthritis and hastens the destruction of the joints involved.
Chondroitin sulfate variants function as signaling molecules and may play essential roles in wound repair and regeneration. The difference between one chondroitin and another is usually the location of negatively charged sulfate groups on a given chondroitin molecule. These differences enable chondroitins to initiate a wide variety of signaling cascades [8].
Chondroitin is connected to glucosamine, hyaluronic acid, and MSM
Glucosamine is naturally made in the human body from glucose and the amino acid glutamine. Glucosamine, in turn, is used to make N-acetyl glucosamine, which is a component of hyaluronic acid. The amount of available glucosamine generally limits the amount of hyaluronic acid that can be made [9].
Hyaluronic acid is a chain of repeating disaccharide subunits made of N-acetyl glucosamine (GlcNAc) and D-glucuronic acid (GlcUA). It provides a backbone to which core proteins are linked. These core proteins, in turn, are linked to large numbers of chondroitin sulfate molecules, as shown [9]. This assembly is referred to as a chondroitin sulfate proteoglycan (CSPG). Studies also indicate that glucosamine and chondroitin sulfate may facilitate hyaluronic acid production [9].
Methylsulfonylmethane (MSM) is often combined with glucosamine chondroitin supplements. Evidence suggests that MSM does two things. First, it increases the expression of genes that support the production of cartilage (chondrogenesis).
Second, it appears to directly and indirectly inhibit NFkB [10], a central mediator of inflammation [11]. Chondroitin prevents NF-kB’s movement from the cytosol into the nucleus, where it drives the expression of genes necessary to produce inflammatory cytokines [5].
Chondroitin performs multiple functions in different organ systems
Chondroitin sulfate influences the health and regenerative capacity of organ systems across the body. Some of these areas include the skin [12], cartilage [13], muscle [14,15], lung [16], gut [17], brain, nerves [18], heart [13], blood vessels [19], and bladder [20].
Cosmetics companies have a long-standing interest in maintaining the youthful appearance of skin. Consequently, scientists in this ndustry have been busy exploring the world for compounds that improve the appearance of skin.
Chondroitin is essential for normal skin health, wound healing and regeneration. A considerable body of research has been dedicated to chondroitin sulfate and related compounds. A recent study looked at changes in gene expression and protein synthesis in skin after the application of chondroitin.
Chondroitin treatment increased the proliferation of cells called keratinocytes, which make up the outermost layer of the skin. Chondroitin also induced the expression of collagen. Using a skin wound model and an aged skin model the research group found that chondroitin promoted wound healing and regeneration in skin [12,21].
Chondroitin sulfate increases cartilage cell proliferation and prevents age-related loss of collagen. Supplementation with chondroitin sulfate increased cartilage cell proliferation in a dose dependent manner in rats. In the model organism C. elegans, chondroitin supplementation slows the progressive decline of collagen renewal [9].
In patient-derived cartilage cells, experiments have shown that chondroitin sulfate supplementation results in the remodeling of ECM proteins and certain inflammatory molecules. Many studies show that chondroitin sulfate supplementation inhibits cartilage destruction and stimulates proteoglycan production for bolstering connective tissues [22].
A review of two meta-analyses suggests that the quality of glucosamine chondroitin supplementation is a vital consideration. Crystalline forms of glucosamine chondroitin appear to be better absorbed and produce better results than non-crystalline forms [23].
Chondroitin sulfate may improve healing and power generation in injured muscle tissue. In injured rat muscle, glucosamine and chondroitin have been shown to improve healing and power generation. This suggests that glucosamine and chondroitin may be useful for the treatment of muscle injuries in human beings [14].
Chondroitin sulfate is present in lung tissue, where it interacts with a wide array of signaling molecules involved in injury, inflammation, and tissue repair. Chondroitin sulfate proteoglycans are present in developing and adult lung tissue as components of the extracellular matrix and basement membrane.
The role of syndecans
Syndecans are a family of proteoglycans that can contain chondroitin as a constituent. They function as membrane receptors and ligand gatherers for an astonishing spectrum of ligands. These molecules work as co-receptors alongside of signaling receptors, acting on such molecules as growth factors, morphogens, and cytokines that are regulators of tissue regeneration. Evidence suggests that syndecans can also signal independently [6]. A growing body of research suggests that syndecans are crucial in normal tissue repair and regeneration [24].
Heparin sulfate proteoglycans, including syndecans, have chondroitin sulfate side chains. Syndecans may also regulate several stem cell properties [16]. Chondroitin is a known constituent of syndecan 1, which plays a complex role in lung inflammatory response to tissue injury [6].
Chondroitin in the gut
Chondroitin supplementation alters the gut microbiome to reduce inflammation and improve gut barrier protection. When chondroitin sulfate is taken as a supplement, only 5%-15% is absorbed from the gut; the other 85%-90% is used by gut bacteria. This raises questions as to how chondroitin sulfate consumption might alter the gut microbiome.
A systematic review of studies focused on the effects of chondroitin on the gut microbiome suggests that some changes in the microbiome do occur. Chondroitin sulfate is used by sulfate-reducing bacteria. These bacteria are involved in the synthesis of anti-inflammatory compounds, whose therapeutic potential is currently under investigation.
Chondroitin is also a component of intestinal mucin, which acts as a barrier between gut flora and the intestinal wall. As such, chondroitin supplementation may affect gut permeability and intestinal immune mediation [17].
Chondroitin supplementation has been shown to increase the relative concentration of some bacterial species and decrease the relative concentration of others. Evidence suggests that the relative changes that occur in the concentration of these bacteria may reduce gut inflammation and improve gut barrier protection [17].
Chondroitin and the nervous system
Chondroitin protects brain tissue from mechanical trauma and regulates pruning and synapse formation. Chondroitin sulfate proteoglycans are a family of molecules made from chondroitin and protein. Different chondroitin variants and variation in the protein structure result in a wide array of chondroitin sulfate proteoglycans, each with unique properties that affect the development and maintenance of the brain and nervous system [3,6].
In the nervous system, chondroitin not only protects nerves from mechanical trauma but also inhibits or encourages connections between neurons. Sometimes, if more extreme damage occurs in the brain, the body may attempt to compensate by overproducing chondroitin which can prevent recovery from traumatic brain injury [18].
Chondroitin and the cardiovascular system
Chondroitin protects the cardiovascular system from mechanical damage and inflammation and reduces cardiovascular disease mortality by 65%. The average person would have to do about 5-8 hours of moderate intensity exercise per week to get a 63% reduction in cardiovascular disease mortality [1,25].
Significant force is produced by the heart to drive blood through the circulatory system. The effects of these forces are more pronounced in individuals with high blood pressure. Chondroitin is present in arterial and heart valve tissue. However, as we age, chondroitin production is reduced and reduced chondroitin production is associated with atherosclerosis.
Chondroitin sulfate has been shown to interfere with the pro-inflammatory and atherogenic effects of TNF-α on monocytes, macrophages, and endothelial cells, which line arterial blood vessel walls [15]. In humans, C-reactive protein levels are lowered in people who take glucosamine chondroitin supplements. C-reactive protein levels, which indicate a propensity toward inflammation, are predictive of cardiac events [9].
Chondroitin and the urinary system
Chondroitin sulfate and hyaluronic acid supplementation may aid in the restoration of the bladder’s mucosal layer to mitigate the effects of bladder disease. The lining of the bladder (bladder epithelium) not only defends against infection but also regulates complex bladder functions.
Strong evidence suggests that the erosion of mucus layer and bladder epithelium marks the beginning of several chronic inflammatory bladder diseases. These diseases include recurrent urinary tract infection (UTI), chemical or radiation cystitis, and painful bladder syndrome/interstitial cystitis (PBS/IC).
Therapeutic use of hyaluronic acid and chondroitin sulfate in a very good study showed a 77% decrease in the UTI rates among women with recurrent UTI infections. Other studies support the use of hyaluronic acid and chondroitin in the treatment of premature bladder emptying, nonbacterial cystitis, and urological malignancies. Further studies are needed to confirm these findings [20].
Chondroitin protects the extracellular matrix
Recent efforts to identify compounds that retard or prevent age-related diseases indicate that most pro-longevity compounds alter the expression of genes that code for proteins in the extracellular matrix (ECM). ECM is the space between cells in tissue.
Major age-related changes in ECM include a progressive decline in collagen, elastin, laminin, and integrin levels coupled with an increase in the activity of extracellular proteases. Proteases are compounds that break down proteins [26].
Genetic alterations in extracellular matrix genes’ expression cause dysfunctional changes in tissue architecture and provoke many age-associated diseases. Many of these diseases are characterized by chronic inflammation and fibrotic collagen deposition [9].
Some of these alterations may be driven by the cellular senescence and the loss of stem cell maintenance. Maintaining collagen expression may be enough to increase the lifespan of certain organisms such as C. elegans. This suggests that ECM protein homeostasis is an unexplored mechanism to promote health during aging [9].
Endogenous chondroitin sulfate is essential for maintaining embryonic stem cell pluripotency via binding to E-cadherin cell adhesion and RhoA and ERK1/2 downstream signaling. Therefore, chondroitin sulfate metabolism is linked to ECM homeostasis.
ECM proteins and remodeling enzymes are well conserved across species. Research suggests that drugs that target proteins associated with the biosynthesis and degradation of chondroitins may help stall aging by enhancing the function of chondroitin throughout the body.
Drug targets would include chondroitinase (GALNS), sulfotransferase (CHST11), chondroitin/hyaluronic acid receptor (CD44), hyaluronidase (HYAL), and enzymes that remodel the ECM, such as the matrix metalloproteinases (MMPs) 1, 3, 16, and 24 [9].
An alternative or complementary approach to drugs would obviously be chondroitin supplementation. Consumption is positively correlated with longevity in several model organisms such as C. elegans roundworms [27].
Pathway analysis of discovered longevity compounds has shown the enrichment of TGFβ, chondroitin, and heparan sulfate biogenesis as potential drug screening targets [28].
Studies addressing the safety and efficacy of glucosamine chondroitin supplementation
Chondroitin is a popular supplement generally consumed with glucosamine with the intention of supporting joint health. Chondroitin hasn’t been analyzed in the same way as a traditional pharmaceutical drug. Therefore, safe upper levels of intake (UL) have not been established, but observed safe levels (OSL) and highest observed intake (HOI) have been.
The OSL risk assessment method indicates that the evidence strongly supports the safety at intakes of up to 2000 mg/day for glucosamine and 1200 mg/day for chondroitin sulfate. The complete absence of side effects at these levels supports the long-term safety of both glucosamine and chondroitin supplements [9,29].
Limited evidence suggests that glucosamine may encourage kidney fibrosis in rare instances. Glucosamine is frequently taken with chondroitin, and the two compounds complement each other. Experimental evidence from animal studies and a limited number of human case studies suggest that glucosamine can, in rare cases, cause apoptosis and overexpression of transforming growth factor β1 (TGF-β1) and connective-tissue growth factor (CTGF) in kidney tissue. These compounds are known to produce fibrosis in kidney tissue [30].
Therefore, individuals with a kidney disease or a genetic predisposition toward kidney disease would be advised to consult with their doctors before taking glucosamine supplements and monitor their kidney function while consuming this supplement.
Glucosamine consumption is not associated with shellfish allergy. Commercial production of glucosamine starts with shellfish, from which chitin is harvested. Shellfish allergy is caused by IgE antibodies to antigens in the flesh of the shellfish and not the shell; therefore, it should be safe for patients with shellfish allergy to take glucosamine supplements [31].
Literature
[1] D. E. King and J. Xiang, “Glucosamine/Chondroitin and Mortality in a US NHANES Cohort,” J. Am. Board Fam. Med., vol. 33, no. 6, pp. 842–847, 2020.
[2] M. Zhao, S. P. Veeranki, C. G. Magnussen, and B. Xi, “Recommended physical activity and all cause and cause specific mortality in US adults: Prospective cohort study,” BMJ, vol. 370, pp. 1–10, 2020.
[3] R. S. Aquino, E. S. Lee, and P. W. Park, “Diverse Functions of Glycosaminoglycans in Infectious Diseases,” in Glycosaminoglycans in Development, Health and Disease, vol. 93, L. B. T.-P. in M. B. and T. S. Zhang, Ed. Academic Press, 2010, pp. 373–394.
[4] C. Kiani, L. Chen, Y. J. Wu, A. J. Yee, and B. B. Yang, “Structure and function of aggrecan,” Cell Res., vol. 12, no. 1, pp. 19–32, 2002.
[5] G. M. Campo, A. Avenoso, S. Campo, A. D’Ascola, P. Traina, and A. Calatroni, “Chondroitin-4-sulphate inhibits NF-kB translocation and caspase activation in collagen-induced arthritis in mice,” Osteoarthr. Cartil., vol. 16, no. 12, pp. 1474–1483, 2008.
[6] J. R. Couchman, “Syndecans: proteoglycan regulators of cell-surface microdomains?,” Nat. Rev. Mol. Cell Biol., vol. 4, no. 12, pp. 926–938, 2003.
[7] A. Aravamudhan, D. M. Ramos, A. A. Nada, and S. G. Kumbar, “Chapter 4 – Natural Polymers: Polysaccharides and Their Derivatives for Biomedical Applications,” S. G. Kumbar, C. T. Laurencin, and M. B. T.-N. and S. B. P. Deng, Eds. Oxford: Elsevier, 2014, pp. 67–89.
[8] V. P. Swarup, T. W. Hsiao, J. Zhang, G. D. Prestwich, B. Kuberan, and V. Hlady, “Exploiting Differential Surface Display of Chondroitin Sulfate Variants for Directing Neuronal Outgrowth,” J. Am. Chem. Soc., vol. 135, no. 36, pp. 13488–13494, Sep. 2013.
[9] C. Y. Ewald, “Drug Screening Implicates Chondroitin Sulfate as a Potential Longevity Pill,” Frontiers in Aging , vol. 2. 2021, [Online].
[10] M. Butawan, R. L. Benjamin, and R. J. Bloomer, “Methylsulfonylmethane: Applications and safety of a novel dietary supplement,” Nutrients, vol. 9, no. 3, pp. 1–21, 2017.
[11] T. Liu, L. Zhang, D. Joo, and S.-C. Sun, “NF-κB signaling in inflammation,” Signal Transduct. Target. Ther., vol. 2, p. 17023, 2017.
[12] D. Min et al., Potential anti-ageing effect of chondroitin sulphate through skin regeneration, vol. 42, no. 5. 2020.
[13] C. D. Koch, C. M. Lee, and S. S. Apte, “Aggrecan in Cardiovascular Development and Disease,” J. Histochem. Cytochem., vol. 68, no. 11, pp. 777–795, 2020.
[14] E. Montell, P. Contreras-Muñoz, A. Torrent, M. de la Varga, G. Rodas, and M. Marotta, “Mechanisms of action of chondroitin sulfate and glucosamine in muscle tissue: in vitro and in vivo results. A new potential treatment for muscle injuries?,” Osteoarthr. Cartil., vol. 26, no. 2018, p. S404, 2018.
[15] P. Melgar-Lesmes et al., “Chondroitin Sulphate Attenuates Atherosclerosis in ApoE Knockout Mice Involving Cellular Regulation of the Inflammatory Response,” Thromb. Haemost., vol. 118, no. 7, pp. 1329–1339, Jul. 2018.
[16] Y. Kai, H. Yoneyama, M. Yoshikawa, H. Kimura, and S. Muro, “Chondroitin sulfate in tissue remodeling: Therapeutic implications for pulmonary fibrosis,” Respir. Investig., vol. 59, no. 5, pp. 576–588, 2021.
[17] A. Shmagel et al., “The Effects of Glucosamine and Chondroitin Sulfate on Gut Microbial Composition: A Systematic Review of Evidence from Animal and Human Studies,” Nutrients, vol. 11, no. 2, p. 294, Jan. 2019.
[18] J. R. Siebert, A. Conta Steencken, and D. J. Osterhout, “Chondroitin sulfate proteoglycans in the nervous system: inhibitors to repair,” Biomed Res. Int., vol. 2014, p. 845323, 2014.
[19] M. B. Keough et al., “An inhibitor of chondroitin sulfate proteoglycan synthesis promotes central nervous system remyelination,” Nat. Commun., vol. 7, 2016.
[20] R. Damiano and A. Cicione, “The role of sodium hyaluronate and sodium chondroitin sulphate in the management of bladder disease,” Ther. Adv. Urol., vol. 3, no. 5, pp. 223–232, 2011.
[21] S. Mishra et al., “Topical application of peptide-chondroitin sulfate nanoparticles allows efficient photoprotection in skin,” ACS Appl. Mater. Interfaces, vol. 13, no. 2, pp. 2382–2398, 2021.
[22] G. Herrero-Beaumont et al., “Glucosamine sulfate in the treatment of knee osteoarthritis symptoms: A randomized, double-blind, placebo-controlled study using acetaminophen as a side comparator,” Arthritis Rheum., vol. 56, no. 2, pp. 555–567, Feb. 2007.
[23] X. Zhu, L. Sang, D. Wu, J. Rong, and L. Jiang, “Effectiveness and safety of glucosamine and chondroitin for the treatment of osteoarthritis: A meta-analysis of randomized controlled trials,” J. Orthop. Surg. Res., vol. 13, no. 1, pp. 1–9, 2018.
[24] H. Chung, H. A. B. Multhaupt, E.-S. Oh, and J. R. Couchman, “Minireview: Syndecans and their crucial roles during tissue regeneration,” FEBS Lett., vol. 590, no. 15, pp. 2408–2417, Aug. 2016.
[25] T. M. H. Eijsvogels, S. Molossi, D. Lee, M. S. Emery, and P. D. Thompson, “Exercise at the Extremes: The Amount of Exercise to Reduce Cardiovascular Events,” J. Am. Coll. Cardiol., vol. 67, no. 3, pp. 316–329, 2016.
[26] C. Statzer et al., “Youthful and age-related matreotypes predict drugs promoting longevity,” Aging Cell, vol. 20, no. 9, pp. 1–14, 2021.
[27] E. J. E. Kim and S.-J. V Lee, “Recent progresses on anti-aging compounds and their targets in Caenorhabditis elegans,” Transl. Med. Aging, vol. 3, pp. 121–124, 2019.
[28] H. Liu, M. Guo, T. Xue, J. Guan, L. Luo, and Z. Zhuang, “Screening lifespan-extending drugs in Caenorhabditis elegans via label propagation on drug-protein networks,” BMC Syst. Biol., vol. 10, no. Suppl 4, 2016.
[29] J. N. Hathcock and A. Shao, “Risk assessment for glucosamine and chondroitin sulfate,” Regul. Toxicol. Pharmacol., vol. 47, no. 1, pp. 78–83, 2007.
[30] S. Gueye, M. Saint-Cricq, M. Coulibaly, N. Goumri, and L. Rostaling, “Chronic tubulointerstitial nephropathy induced by glucosamine: a case report and literature review.,” Clin. Nephrol., vol. 86, pp. 106–110, 2016.
[31] H. C. Gray, P. S. Hutcheson, and R. G. Slavin, “Is glucosamine safe in patients with seafood allergy?,” J. Allergy Clin. Immunol., vol. 114, no. 2, pp. 459–460, Aug. 2004.


