A Senolytic Approach to Faster Wound Healing
- This approach encouraged potentially helpful infammation.

Researchers have published in Aging their findings that a senolytic compound accelerates wound healing in aged mice when it is administered before the wound occurs.
A well-known laboratory senolytic
While some senescent cells have been found to have a beneficial effect on wound healing [1], the increase in cellular senescence with age has been suspected of slowing down healing instead [2]. ABT-263 is a senolytic compound that has been commonly researched in the laboratory, and previous work has found that it reduces some of the signs of skin aging [3]. Therefore, this research was a straightforward logical progression, although some of the findings were counterintuitive.
In their first experiment, the researchers treated the skin of 24-month-old mice with either DMSO, a compound that helps to infuse other compounds into the skin, by itself (control group) or a combination of DMSO and ABT-263 (treatment group) for five days. This corroborated other research showing ABT-263’s senolytic effects, as the treatment group’s skin had less of the senescence markers p16 and p21 along with the senescence biomarker SA-β-gal. These findings only applied in an aged population, as they were not replicated in 2-month-old mice.
Intriguing but positive effects
Despite these senolytic effects, the treatment increased, not decreased, inflammation as a whole. Compared to DMSO alone, 24-month-old mice that received the treatment had significantly increased macrophage infiltration of the skin, and there was an elevation in neutrophils as well. However, they also had significanty fewer T cells.
The researchers hypothesize that this is due to mass senolysis: the senescent cells, dying in large quantities, release their contents into the area, and these damage-associated molecular pattern (DAMPs) spur macrophages to clean up their remains. This is in line with previous work showing that transient inflammation may accelerate wound heaing [4].
The researchers note that ABT-263 is known to spur senescent cell removal (senolysis) by inhibiting the Bcl-2 protein family, which prevents cells from dying by apoptosis. Those findings were replicated in this study: Bcl2 was significantly upregulated in the treatment group.
Interestingly, some but not all of the SASP, which is secreted by senescent cells, was upregulated by ABT-263 compared to controls. A database of SASP genes expressed in mice did not find any significant differences as a whole. However, many inflammatory factors, including interleukins and chemokines, that previous work had found to be associated with the SASP [5] were very significantly upregulated by ABT-263.
Most critically for this study, genes related to wound healing were also significantly upregulated by the treatment. The expression of genes related to blood vessel formation, collagen synthesis, and cellular proliferation were increased alongside inflammation and wound healing more generally.
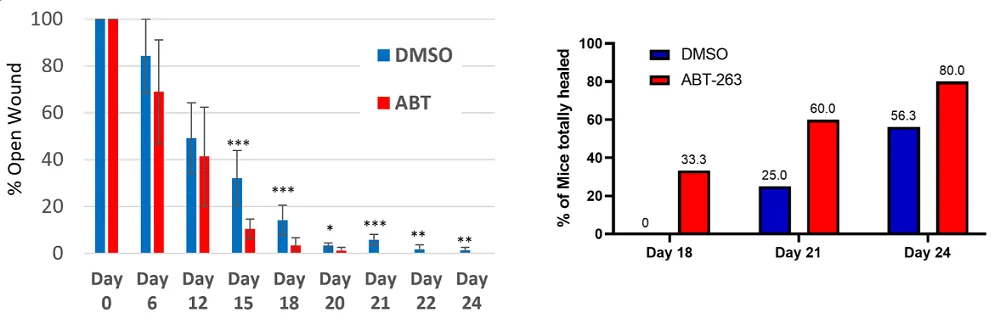
Pre-treating aged mouse skin with ABT-263 before a wound was inflicted yielded fruitful results. Here, 24-month-old mice were treated with either the DMSO control or the active combination for five days before a one centimeter-wide patch of skin was cut away. By day 15, the treatment’s effects were statistically significant: a third of the treatment group was considered to be totally healed, while none of the control group met this threshold. By day 21, the treated mice had no open wounds remaining, while some of the untreated mice still had visible injuries.
Is a topical approach best?
The researchers note some differences between their approach, which only applied ABT-263 to small patches of skin, and previous work that introduced ABT-263 to mice more systemically. There was a risk of a loss of neutrophils (neutropenia), but this topical approach increased neutrophils instead. Furthermore, the pretreatment-only approach they used was intentional; they noted the role of senescent cells in wound healing and the potential risk in removing them once healing had begun.
Therefore, it is unlikely that ABT-263 will ever be employed as an after-the-fact wound treatment. However, it holds promise for surgery, which involves pre-planned wounds. If older people with more senescent skin are given topical ABT-263 before these sorts of medical interventions, such a treatment could potentially reduce their recovery time and encourage healthy collagen production; however, it remains to be seen if the murine findings of this study apply to human beings.
Literature
[1] Kim, H., Jang, J., Song, M. J., Kim, G., Park, C. H., Lee, D. H., … & Chung, J. H. (2022). Attenuation of intrinsic ageing of the skin via elimination of senescent dermal fibroblasts with senolytic drugs. Journal of the European Academy of Dermatology and Venereology, 36(7), 1125-1135.
[2] Andrade, A. M., Sun, M., Gasek, N. S., Hargis, G. R., Sharafieh, R., & Xu, M. (2022). Role of senescent cells in cutaneous wound healing. Biology, 11(12), 1731.
[3] Kita, A., Yamamoto, S., Saito, Y., & Chikenji, T. S. (2024). Cellular senescence and wound healing in aged and diabetic skin. Frontiers in Physiology, 15, 1344116.
[4] Naik, S., Larsen, S. B., Gomez, N. C., Alaverdyan, K., Sendoel, A., Yuan, S., … & Fuchs, E. (2017). Inflammatory memory sensitizes skin epithelial stem cells to tissue damage. Nature, 550(7677), 475-480.
[5] Coppé, J. P., Desprez, P. Y., Krtolica, A., & Campisi, J. (2010). The senescence-associated secretory phenotype: the dark side of tumor suppression. Annual review of pathology: mechanisms of disease, 5(1), 99-118.







