Does WHO 5 Year Plan Leave Healthy Aging Out of the Picture?

When it comes to healthcare, WHO remains the global flagship in terms of setting priorities and adjusting policies in the ever-changing landscape of healthcare needs. In the past few years, WHO has been making steps towards preparing our society to handle the “silver tsunami” and the increasing needs of the elderly population, which is expected to reach 22% of the global population by 2050.
The last 12th General Programme of Work, adopted by the World Health Assembly in May 2013, listed population aging and morbidity of age-related diseases as one of the points of great concern. However, in the recent Draft thirteenth general programme of work 2019–2023, the priorities related to aging and age-related disease are… gone.
What is this, a tragic accident or the worst example of ageism at the level of the global policymaking? Can the Open Consultation running until November 15 help bring healthy aging back into the WHO agenda? You will also find The LEAF Position regarding the Draft programme at the end of this article, but first, let’s discuss why this is important to keep healthy aging among the top priorities.
After all the efforts to introduce aging and the problems of the growing share of the elderly into the international agenda, WHO seems to fall back by 30 years and leave this most important question out the discourse for the next 5 years. While the Draft thirteenth general programme of work 2019–2023 claims to be based on the Sustainable Development Goals, it is clear that it is throwing out the problems of the elderly. For instance, the SDG indicated the need to promote the development and implementation of medicines against noncommunicable diseases; this never made it to the new draft, and neither did the four main diseases with the highest mortality rates. Here are the quotes from the SDG indicators:
3.4
By 2030, reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being
3.4.1
Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease …
3.B Support the research and development of vaccines and medicines for the communicable and non-communicable diseases that primarily affect developing countries, provide access to affordable essential medicines and vaccines, in accordance with the Doha Declaration on the TRIPS Agreement and Public Health, which affirms the right of developing countries to use to the full the provisions in the Agreement on Trade-Related Aspects of Intellectual Property Rights regarding flexibilities to protect public health, and, in particular, provide access to medicines for all.
The priorities of the new draft moved elsewhere and do not pay much attention to age-related diseases, which account for most deaths among the ones caused by NCDs. Here is how the set of priorities on NCDs is formulated in the draft:
3. Noncommunicable diseases (NCDs), mental health, substance use, road traffic injuries- Reduce tobacco use by 25%
- Reduce harmful alcohol use by 10% (per capita consumption)
- Keep the levels stable for overweight (including obesity) in children and adolescents
- Eliminate industrially produced trans fats
- Reduce prevalence of raised blood pressure by 20%
- Increase service coverage for severe mental health disorders by 40 percentage points
- Reduce road traffic fatalities by 20%
This list is barely touching upon age-related health issues (high blood pressure is probably the most relevant point), while the priorities 1, 2 and 4 are completely different. Looking at this document, we are desperately asking ourselves why WHO is suddenly turning its back on the elderly population and what we shall expect to happen to the previous strategic programs, as the draft mentions that it will also influence the Programme budget of 2018−2019 through a mechanism of resource reallocation. Should we treat it as a warning that the resources previously expected to help fulfill the Global strategy and plan of action on ageing and health are going to be redirected to this new “ageist” set of goals?
WHO is currently running an open public consultation on the draft, and we invite you to take part and provide your view regarding the necessity of keeping the issue of age-related diseases in the WHO agenda in the years to come. However, before we provide you with the position that we are going to send to WHO (the example is at the end of this article), we would like to remind you of the key indicators and documents with which you should be familiar in order to make an informed decision regarding the global healthcare agenda.
The age group 60+ is growing faster than any other
The global population is aging rapidly. Here is a quote from the UN Population Prospects 2017 Revision Key Findings concerning this change:
In 2017, there are an estimated 962 million people aged 60 or over in the world, comprising 13 per cent of the global population. The population aged 60 or above is growing at a rate of about 3 per cent per year. Currently, Europe has the greatest percentage of population aged 60 or over (25 per cent). Rapid ageing will occur in other parts of the world as well, so that by 2050 all regions of the world except Africa will have nearly a quarter or more of their populations at ages 60 and above. The number of older persons in the world is projected to be 1.4 billion in 2030 and 2.1 billion in 2050, and could rise to 3.1 billion in 2100. Over the next few decades, a further increase in the population of older persons is almost inevitable, given the size of the cohorts born in recent decades.NCDs disproportionately affect people in low- and middle-income countries
Worldwide, infectious diseases have been replaced by chronic non-communicable diseases (NCDs) as the leading causes of death; this is called the epidemiological transition. This transition is associated with the most developed countries, but this is a widespread misconception. According to WHO, NCDs disproportionately affect people in low- and middle-income countries, where more than three-quarters of global NCD deaths – 31 million annually – occur. The most frequent NCDs are cardiovascular diseases (heart attacks and stroke), cancers, chronic respiratory diseases (such as COPD), and diabetes. Here is the quote from the WHO fact sheet regarding NCDs:
Cardiovascular diseases account for most NCD deaths, or 17.7 million people annually, followed by cancers (8.8 million), respiratory diseases (3.9 million), and diabetes (1.6 million).
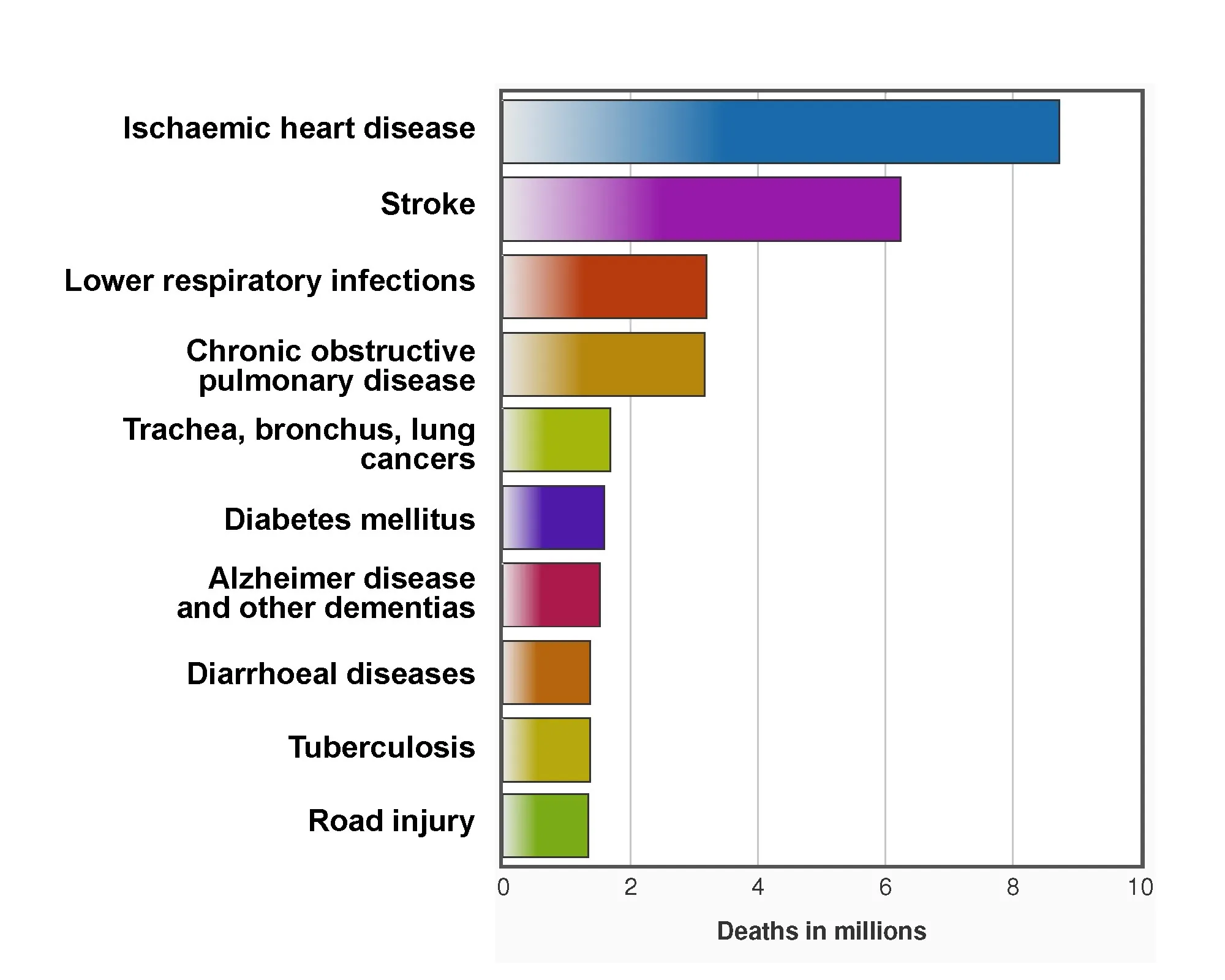
Chronic diseases make most of the top 10 causes of death globally
If we look at the WHO estimates of the main causes of death globally, we can see that age-related chronic diseases account for the vast majority of deaths, with infectious diseases and road injury comprising a much smaller part:
Most recent WHO strategic documents are focused on age-related issues
This data on population aging, combined with the data on morbidity, informed the previous WHO activities related to aging. In 2015, it released the World report on ageing and health, creating an exhaustive overview of population aging, discussing related health, social and economic changes, and describing the necessary actions to make the older population as healthy as possible. The report set the following definition of healthy aging and its mandatory elements:
Healthy Ageing is the process of developing and maintaining the functional ability that enables well-being in older age.
Functional ability comprises the health-related attributes that enable people to be and to do what they have reason to value. It is made up of the intrinsic capacity of the individual, relevant environmental characteristics and the interactions between the individual and these characteristics.
Intrinsic capacity is the composite of all the physical and mental capacities of an individual.
Environments comprise all the factors in the extrinsic world that form the context of an individual’s life. These include – from the micro-level to the macro-level – home, communities and the broader society. Within these environments are a range of factors, including the built environment, people and their relationships, attitudes, and values, health and social policies, the systems that support them, and the services that they implement.
Well-being is considered in the broadest sense and includes domains such as happiness, satisfaction and fulfilment.Based on the indicators listed in this report, the Global strategy and plan of action on ageing and health was developed and signed into power in 2016, setting the following strategic objectives and goals to prepare for the Decade of Healthy Aging (2020-2030):
VISION A world in which everyone can live a long and healthy life
STRATEGIC OBJECTIVES 1. Commitment to action on Healthy Ageing in every country 2. Developing age-friendly environments 3. Aligning health systems to the needs of older populations 4. Developing sustainable and equitable systems for providing long-term care (home, communities and institutions) 5. Improving measurement, monitoring and research on Healthy Ageing
PLAN OF ACTION 2016–2020
GOALS 1. Five years of evidence-based action to maximize functional ability that reaches every person. 2. By 2020, establish evidence and partnerships necessary to support a Decade of Healthy Ageing from 2020 to 2030.
This document also points out the need to support the development of innovative interventions to address age-related diseases and their underlying causes:
- Finally, better clinical research is urgently needed on the etiology of, and treatments for, the key health conditions of older age, including musculoskeletal and sensory impairments, cardiovascular disease and risk factors such as hypertension and diabetes, mental disorders, dementia and cognitive declines, cancer, and geriatric syndromes such as frailty. This must include much better consideration of the specific physiological differences of older men and women and the high likelihood that they will be experiencing multimorbidities. This could also be extended to include possible interventions to modify the underlying physiological and psychological changes associated with ageing.
The LEAF Position regarding the Draft thirteenth general programme of work 2019–2023
Taking this information into account, we suggest the following position regarding the Draft thirteenth general programme of work 2019–2023 that can provide insight and inspiration for your own position. The Open Consultation will be running until November 15. To take part and share your vision with WHO, please visit this WHO page, scroll down, and fill the mandatory fields of the survey.
- The global population is aging rapidly, and according to the UN Population Prospects 2017 Revision, the share of people aged 60+ will make up 22% of the global population by 2050[a]. Sadly, higher life expectancy does not necessarily mean an extension of the healthy period of life, and more people around the globe live longer while suffering from chronic age-related diseases, with the developing countries bearing the most burden.
- Most countries already experience epidemiological transition, with non-communicable diseases, particularly age-related diseases, becoming leading causes of death. The most frequent NCDs are cardiovascular diseases (heart attacks and stroke), cancers, chronic respiratory diseases (such as COPD) and diabetes. Cardiovascular diseases account for most NCD deaths, or 17.7 million people annually, followed by cancers (8.8 million), respiratory diseases (3.9 million), and diabetes (1.6 million)[b].
- The Sustainable Development Goals set the goal to “reduce mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease” (3.4.1), and to “support the research and development of vaccines and medicines for the communicable and noncommunicable diseases that primarily affect developing countries, provide access to affordable essential medicines and vaccines…” (3.B).
- The latest WHO World report on ageing and health (2015) and the Global strategy and plan of action on ageing and health (2016) underline the need to promote healthy aging for all, and they recommend the corresponding set of measures, including better clinical research on the etiology of, and treatments for, the key health conditions of older age, including musculoskeletal and sensory impairments, cardiovascular disease and risk factors such as hypertension and diabetes, mental disorders, dementia and cognitive declines, cancer, and geriatric syndromes such as frailty, along with possible interventions to modify the underlying physiological and psychological changes associated with aging (with consideration of the specific physiological differences of older men and women and the high likelihood that they will be experiencing multimorbidities)[c].
- Clinical trials of several innovative interventions that can address the underlying mechanisms of aging, postpone and cure age-related diseases, and extend the healthy period of life (senolytics, thymus regeneration in situ, therapies to regulate NAD+ and improve DNA repair, metformin) are currently being performed, and these interventions can enter the market in the next 5 years. WHO supervision and guidance regarding the implementation of these interventions is required to ensure their rapid, worldwide dissemination, affordability and equal access.
- While we recognize the need to promote universal health coverage, to keep fighting infectious diseases and mental illnesses, and to promote the health of women, children and adolescents, we find efforts to ensure healthy aging to be of vital importance for our society’s well-being in the decades to come. If this most important topic will be excluded from the global agenda, and the corresponding funding reallocated to solve other health issues, not only it will be an unhealthy example of ageism at the highest level of policymaking, but our society will also face the growing needs of the increasing older population unprepared and disoriented.
- The global and local effects of not addressing these issues can be devastating, posing an increasing burden on healthcare and social protection systems (for instance, public health expenditures in the United States are projected to rise from 6.7 percent of GDP in 2010 to 14.9 percent in the year 2050), causing shortages of professional caregivers for aged patients, which will turn a significant part of the working population into compulsory family caregivers and undermine sustainable economic growth.
- In order to extend good health and productivity throughout the life course and to ensure that older people preserve their intrinsic ability for as long as possible, we need to keep working in the directions set by the Global strategy and plan of action on ageing and health (2016), including the promotion of clinical research on possible interventions to modify the underlying physiological and psychological changes associated with aging. Hence, we kindly ask you to include promoting healthy aging as a priority of the Draft thirteenth general programme of work 2019–2023.
[a] United Nations, Department of Economic and Social Affairs, Population Division (2017). World Population Prospects: The 2017 Revision, Key Findings and Advance Tables. Working Paper No. ESA/P/WP/248.
[b] WHO. The top 10 causes of death. Fact sheet. Updated January 2017.
[c] WHO Global Strategy and Action Plan on Ageing and Health,” World Health Organization, accessed November 8, 2017.
Thank you very much for finding time to fill out this survey!
Providing policymakers like WHO with our vision regarding the potential of rejuvenation technologies to tackle the problems related to population aging is very important. This way, we help disseminate information about rejuvenation biotechnologies in our society while we encourage more people to support researchers and to start using the interventions that are already available.
We would like to thank Dr. Ilia Stambler for bringing this matter to our attention.







