The Link Between NAD+ and Heart Failure
- An epigenetic regulator impacts how well mitochondria perform.

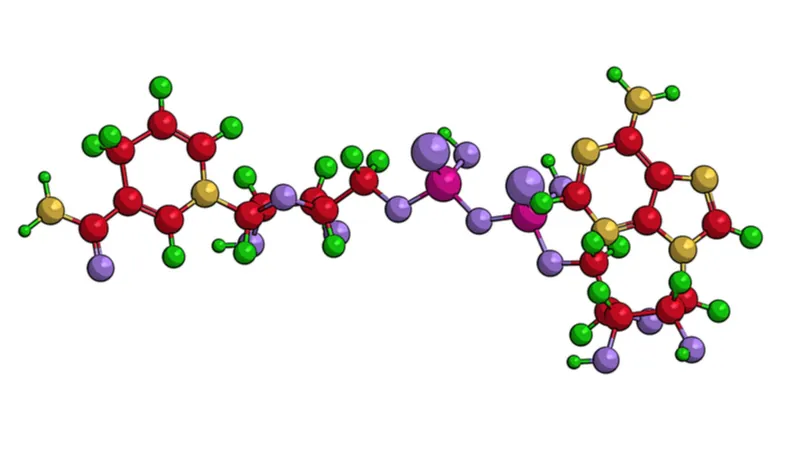
A paper published today in Nature Cardiovascular Research has explained a relationship between dilated cardiac myopathy (DCM), epigenetic dysregulation, NAD+, and the epigenetic regulatory molecule Kdm8.
A gradual decline of ability
DCM occurs when the left ventricle of the heart becomes enlarged and loses its ability to pump enough blood. The heart muscle gradually thins, causing additional mechanical stress, and this leads to cell death [1] and fibrosis [2]. This makes it the primary reason for heart transplantation [3], as this condition slowly leads to heart failure [4].
The mitochondria of the heart muscle cells (cardiomyocytes) are negatively affected by this condition as well, and their ability to process food and oxygen declines; the powerhouses of the cell lose their power [5]. The resulting depletion of ATP is a key component of DCM’s severity [6]. Previous studies have shown that introducing NAD+ to mice afflicted by this condition restores their heart function [7].
Read More
Histone methyltransferases and demethylases, which regulate epigenetics, have been reported to have significant impacts on cardiac function [8]. This research focuses on lysine demethylase 8 (Kdm8), without which mouse embryos die of heart failure before they are born [9]. Previous experiments, however, have not examined the effects of this regulator on living mouse hearts.
Mice with reduced Kdm8 develop DCM
To test their hypothesis, the researchers developed a mouse crossbreed with the KDM8 gene heavily downregulated, most notably in the cardiomyocytes. These mice had relatively normal hearts at 2 months of age but began to show signs of DCM at 4 and 6 months. Mice with two copies of the mutation lived shorter lives (median 7.3 months) than mice with one copy (median 9.3 months), and their deaths were due to heart failure. Mice with no copies of the gene, but which had a different mutation due to the experimental procedure, lived for 27.3 months on average.
As expected, genes related to mitochondrial oxidation were heavily downregulated in the mutants compared to the control group. Mice with one copy of the mutation had more mitochondria, but they were much smaller. Further examination of gene methylation showed that the Kdm8-depleted cardiomyocytes had widespread dysregulation in many other aspects as well, most notably NAD+ metabolism.
Multiple aspects of NAD+, including both its creation and consumption, were heavily downregulated with the loss of Kdm8. This included both NAMPT and the well-known sirtuins, which have been associated with longevity. At 6 months of age, available ATP was roughly half that of controls.
These results proved the researchers’ basic hypothesis: that Kdm8 is a critical component of mitochondrial energy use in cardiomyocytes, which strongly affects heart function.
Conclusion
While this study was not conducted from the point of view of aging research, it touches upon a critical aspect. It has long been known that sirtuins and NAD+ metabolism decline with aging, which is part of deregulated nutrient sensing and heavily related to mitochondrial dysfunction. This in-depth paper describes a specific way in which this depletion appears to be related to epigenetic alterations as well. While potential treatments were not explored in this study, it may be that Kdm8 is a worthwhile target for restoring metabolic ability to the aging heart.
Literature
[1] Aharinejad, S., Andrukhova, O., Lucas, T., Zuckermann, A., Wieselthaler, G., Wolner, E., & Grimm, M. (2008). Programmed cell death in idiopathic dilated cardiomyopathy is mediated by suppression of the apoptosis inhibitor Apollon. The Annals of thoracic surgery, 86(1), 109-114.
[2] Agapitos, E., Kavantzas, N., Nanas, J., Margari, Z., Bakouris, M., Kassis, K., … & Davaris, P. (1996). The myocardial fibrosis in patients with dilated cardiomyopathy. The application of image analysis in the myocardial biopsies. General & diagnostic pathology, 141(5-6), 305-311.
[3] Manolio, T. A., Baughman, K. L., Rodeheffer, R., Pearson, T. A., Bristow, J. D., Michels, V. V., … & Harlan, W. R. (1992). Prevalence and etiology of idiopathic dilated cardiomyopathy (summary of a National Heart, Lung, and Blood Institute workshop). The American journal of cardiology, 69(17), 1458-1466.
[4] McNally, E. M., & Mestroni, L. (2017). Dilated cardiomyopathy: genetic determinants and mechanisms. Circulation research, 121(7), 731-748.
[5] Dávila-Román, V. G., Vedala, G., Herrero, P., De Las Fuentes, L., Rogers, J. G., Kelly, D. P., & Gropler, R. J. (2002). Altered myocardial fatty acid and glucose metabolism in idiopathic dilated cardiomyopathy. Journal of the American College of Cardiology, 40(2), 271-277.
[6] Lopaschuk, G. D., Karwi, Q. G., Tian, R., Wende, A. R., & Abel, E. D. (2021). Cardiac energy metabolism in heart failure. Circulation research, 128(10), 1487-1513.
[7] Diguet, N., Trammell, S. A., Tannous, C., Deloux, R., Piquereau, J., Mougenot, N., … & Mericskay, M. (2018). Nicotinamide riboside preserves cardiac function in a mouse model of dilated cardiomyopathy. Circulation, 137(21), 2256-2273.
[8] Davis, K., Azarcon, P., Hickenlooper, S., Bia, R., Horiuchi, E., Szulik, M. W., & Franklin, S. (2021). The role of demethylases in cardiac development and disease. Journal of Molecular and Cellular Cardiology, 158, 89-100.
[9] Ishimura, A., Minehata, K. I., Terashima, M., Kondoh, G., Hara, T., & Suzuki, T. (2012). Jmjd5, an H3K36me2 histone demethylase, modulates embryonic cell proliferation through the regulation of Cdkn1a expression. Development, 139(4), 749-759.







