Mutation-Carrying CAR T Cells Eradicate Cancer in Mice
- It might be possible to harness cancer to beat cancer.
Scientists have found that giving CAR T cells a particular oncogenic mutation greatly improves their efficiency against blood and solid cancers [1].
Less than cancer
One reason why cancer is so dangerous is that oncogenic mutations boost cancer cells’ survivability, just like a genetically modified monster in a sci-fi movie. When T cells go haywire like that, they cause cancers such as leukemias and lymphomas.
On the other hand, it is practically impossible for cancer to be caused by a single mutation. To become cancerous, cells need to undergo several mutations [2]. What if we could pick one that increases T cells’ fitness but, on its own, does not make them cancerous – and apply this mutation to chimeric antigen receptor (CAR) T cells that have already been modified to attack cancer? This was the reasoning behind a new study published in Nature.
Genomic fusion
The researchers created a library of 71 mutations and introduced them into human and mouse CAR T cells to assess how each one of those mutations affects the cells’ phenotype. After examining various metrics of T-cell fitness and aggressiveness in culture and then in a mouse model of leukemia, the researchers singled out a rare mutation, previously only reported in one lymphoma patient, called CARD11–PIK3R3.
The notation means this is a fusion of two genes, rather than a point mutation, in which a single nucleotide gets replaced or deleted [3]. Gene fusion happens when two or more genes, originally located separately on the genome, are joined by a chromosomal rearrangement such as translocation, deletion, or inversion. When genes fuse, the proteins they encode can also become fused, affecting their normal function or regulation.
Impressive synergy
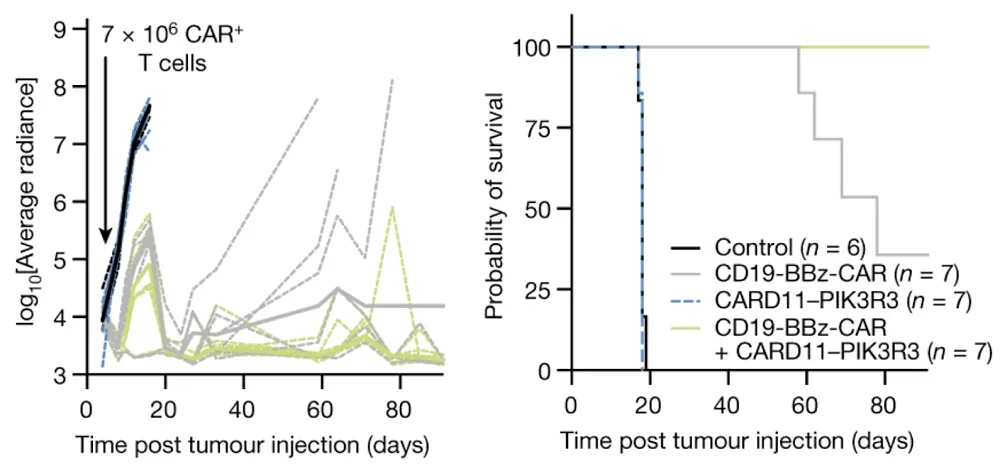
CARD11–PIK3R3 enhanced the production of the cytokines NF-κB and IL-2, which play important roles in their ability to kill target cells (T cell cytotoxicity), but did not cause uncontrolled proliferation. However, the effect was dependent on CAR stimulation – that is, it only worked if CAR T cells carrying the mutation encountered cancerous cells carrying the antigen.
The researchers then experimented with several types of blood and solid cancer, pitting mutation-carrying CAR T cells against regular CAR T cells that are currently used to treat those cancers. In all cases, the combination of the mutation and the CAR vastly outperformed cells carrying either one, resulting in complete or nearly complete survival.
The new therapy’s advantage was especially noticeable with low doses. While normally, CAR T therapies require injecting millions of T cells per kilogram of weight, much fewer of the mutation-carrying CAR T cells were enough to eradicate cancer. This is important since expansion of T cells prior to their injection can lead to exhaustion or senescence. The fewer the number of divisions the cells undergo, the fitter they potentially are.
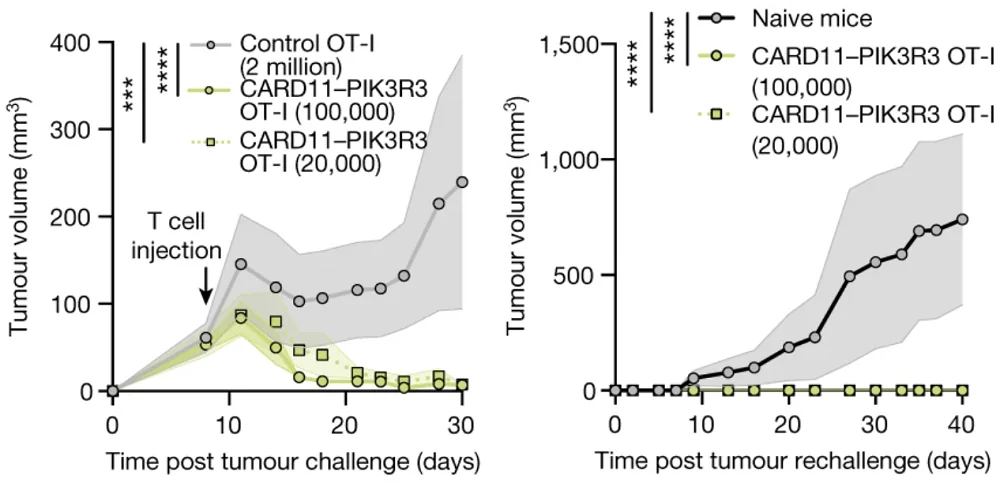
The researchers also experimented with T cell receptor (TCR) cells, a newer approach that uses a different kind of receptor [4]. TCR technology has yet to reach clinics, but it is considered highly promising for the treatment of solid cancers. In a melanoma model, an injection of just 20,000 mutation-carrying TCR cells was just as effective as 100,000 TCR cells without the mutation and led to a complete response in all cases.
Even at high doses, the treated animals gained weight after the injection, showing that the therapy was safe and well-tolerated. Importantly, the impressive therapeutic effect was achieved without reducing the number of lymphocytes in the body (lymphodepletion), which is often used to enhance CAR T cell therapy but can have detrimental health effects.
By screening T cell neoplasm mutations through both in vitro and in vivo arrayed assays, we identified how individual mutations can tune T cell signalling, improve cytotoxic T cell functions and promote in vivo accumulation. This approach identified a new gene fusion, CARD11–PIK3R3, which markedly enhances therapeutic T cell function and efficacy. CARD11–PIK3R3, although discovered in a CD4+ T cell lymphoma, had outsized effects in CD8+ T cells, increasing function in vitro and tumour control in vivo in xenograft and syngeneic models. Future work is required to better understand the mechanistic differences of CARD11–PIK3R3 signalling in CD4+ and CD8+ T cells, as well as PIK3R3 targets in CARD11–PIK3R3-expressing cells.
Literature
[1] Garcia, J., Daniels, J., Lee, Y. et al. Naturally occurring T cell mutations enhance engineered T cell therapies. Nature (2024).
[2] Anandakrishnan, R., Varghese, R. T., Kinney, N. A., & Garner, H. R. (2019). Estimating the number of genetic mutations (hits) required for carcinogenesis based on the distribution of somatic mutations. PLoS computational biology, 15(3), e1006881.
[3] Taniue, K., & Akimitsu, N. (2021). Fusion genes and RNAs in cancer development. Non-coding RNA, 7(1), 10.
[4] Tsimberidou, A. M., Van Morris, K., Vo, H. H., Eck, S., Lin, Y. F., Rivas, J. M., & Andersson, B. S. (2021). T-cell receptor-based therapy: An innovative therapeutic approach for solid tumors. Journal of Hematology & Oncology, 14(1), 1-22.