Niacin Increases NAD+ Significantly in Human Trial

Researchers have concluded a human trial using niacin, a very old vitamin discovered over 80 years ago, and have shown that it can increase the presence of an energy compound essential to cellular function.
Niacin and NAD+
Niacin is a form of water-soluble vitamin B3 and has been known since American biochemist Conrad Elvehjem identified it in 1937. Niacin was originally called nicotinic acid because it can be created by the oxidation of nicotine with nitric acid. However, people know nicotine to be the addictive chemical in tobacco, so the name niacin was adopted, which comes from the words NIcotinic ACid vitamIN.
There has been considerable interest in supplements that have the ability to increase NAD+ levels in recent years, and niacin is one such supplement that can do this. NAD+ biology plays an important role in energy metabolism, so before we dive into the results of a new human study that we want to spotlight today, we should discuss NAD+ and why it is important in the context of metabolism and aging.
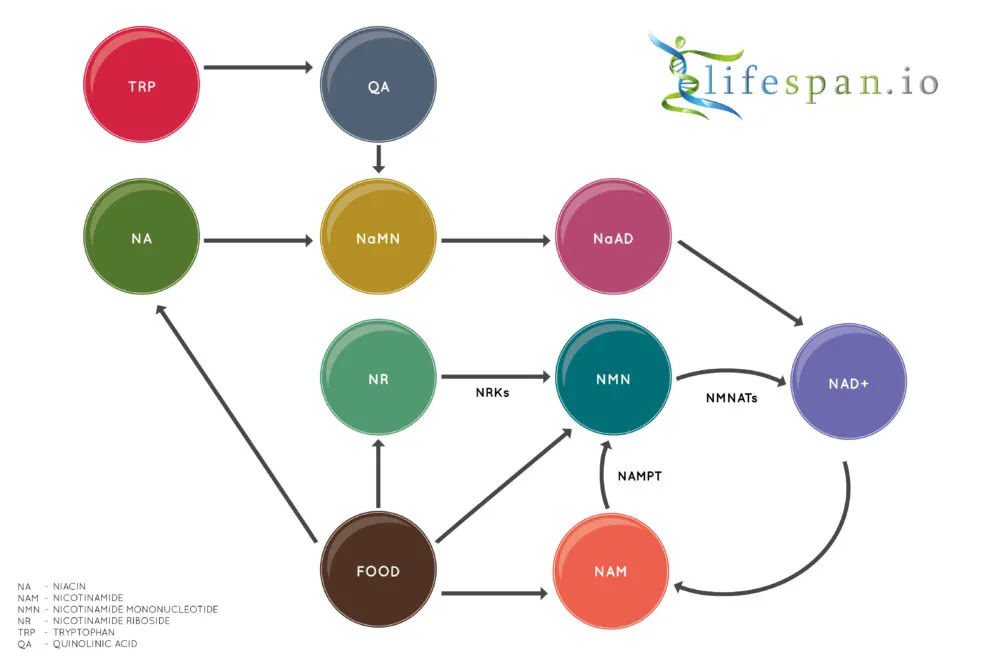
Nicotinamide adenine dinucleotide (NAD) is a coenzyme found in all living cells. It is a dinucleotide, which means that it consists of two nucleotides joined through their phosphate groups. One nucleotide contains an adenine base, and the other contains nicotinamide.
In metabolism, NAD facilitates redox reactions, carrying electrons from one reaction to another. This means that NAD is found in two forms in the cell; NAD+ is an oxidizing agent that takes electrons from other molecules in order to become its reduced form, NADH. NADH can then become a reducing agent that donates the electrons it carries. The transfer of electrons is one of the main functions of NAD, though it also performs other cellular processes, including acting as a substrate for enzymes that add or remove chemical groups from proteins in post-translational modifications.
NAD+ is created from simple building blocks, such as the amino acid tryptophan, and it is created in a more complex way via the intake of food that contains nicotinic acid (niacin) or other NAD+ precursors. These different pathways ultimately feed into a salvage pathway, which recycles them back into the active NAD+ form.
An old compound given a new lease of life
The results of a new human trial using niacin shed new light on its role in NAD+ biology [1].
The trial participants were given a steadily increasing dose of niacin, starting at 250 mg/day to 750-1000 mg/day over a 4-month period, then a 10-month follow-up treatment period. The participants were organized into a study group of individuals with mitochondrial myopathy and a control group of healthy age-matched people consisting of two healthy people for each patient with mitochondrial myopathy. All the study participants were placed on the same niacin supplementation regimen.
The researchers report that niacin treatment increased muscle NAD+ levels by 1.3-fold at 4 months and 2.3-fold after 10 months in the study group. The control group saw no increase of NAD+, suggesting its levels are highly controlled in skeletal muscle tissue and will only increase in patients suffering from lower than normal levels of NAD+ experienced in conditions such as mitochondrial myopathy and potentially aging which also effects mitochondrial fuction. This is also important, as prior to this study, it was unknown if niacin supplementation improved NAD+ in muscle or if it is filtered out and simply elevated NAD+ in the liver.
The level of whole blood NAD+ was also increased by supplementation by 7.1-fold in the study group and 5.7 in the control group after 4 months compared to the participants’ baseline. At the 10-month mark, the increase was 8.2-fold compared to the baseline. This shows that niacin supplements are not simply filtered out by the liver; in fact, they reach the bloodstream in significant amounts to elevate NAD+ levels there.
Niacin supplementation also appears to improve body composition. Participants saw a decrease in whole-body fat percentage in controls and increased muscle mass in both the control and study group. After 10 months of niacin supplementation, the patients demonstrated improved muscle strength.
The researchers also observed that hepatic fat was halved and visceral fat was reduced by a quarter. These types of fat deposits are both linked to an increased risk of metabolic syndrome. So while the niacin had no effect on the surface fat around the body, it did impact significantly on the unhealthy fat surrounding the organs.
Finally, niacin has been linked to increasing blood glucose levels, a risk factor for developing conditions such as diabetes. The results of the study showed that niacin did increase fasting glucose levels in both study and control groups following 4 months of supplementation. However, glycosylated hemoglobin, which reflects long-term glucose levels, was not affected.
So, while niacin does appear to increase glucose levels according to the results of this study, the benefits appear to significantly outweigh any negatives that a slight elevation of glucose may have, as other studies support [2].
The other side effect of note following 4 months of niacin supplementation was that there was a slight decrease in hemoglobin concentration in the participants; however, this never fell below normal healthy ranges during the study.
NAD+ is a redox-active metabolite, the depletion of which has been proposed to promote aging and degenerative diseases in rodents. However, whether NAD+ depletion occurs in patients with degenerative disorders and whether NAD+ repletion improves their symptoms has remained open. Here, we report systemic NAD+ deficiency in adult-onset mitochondrial myopathy patients. We administered an increasing dose of NAD+-booster niacin, a vitamin B3 form (to 750-1,000 mg/day; clinicaltrials.gov NCT03973203) for patients and their matched controls for 10 or 4 months, respectively. Blood NAD+ increased in all subjects, up to 8-fold, and muscle NAD+ of patients reached the level of their controls. Some patients showed anemia tendency, while muscle strength and mitochondrial biogenesis increased in all subjects. In patients, muscle metabolome shifted toward controls and liver fat decreased even 50%. Our evidence indicates that blood analysis is useful in identifying NAD+ deficiency and points niacin to be an efficient NAD+ booster for treating mitochondrial myopathy.
Conclusion
These results give food for thought when we consider NAD+ biology in the context of metabolism and aging. The price of other precursor supplements that may increase NAD+ in humans, such as NR and NMN, are very high compared to niacin, which is cheap and readily available. These results show that niacin can elevate human NAD+ in muscle and blood and potentially in other tissues as well.
Needless to say, while these results are intriguing, we do not endorse supplement use or any product or supplement vendor, and all discussion here is for scientific interest.
Literature
[1] Pirinen, E., Auranen, M., Khan, N. A., Brilhante, V., Urho, N., Pessia, A., … & Haimilahti, K. (2020). Niacin cures systemic NAD+ deficiency and improves muscle performance in adult-onset mitochondrial myopathy. Cell Metabolism.
[2] Goldberg, R. B., & Jacobson, T. A. (2008, April). Effects of niacin on glucose control in patients with dyslipidemia. In Mayo Clinic Proceedings (Vol. 83, No. 4, pp. 470-478). Elsevier.