Taking Up Exercise Late in Life May Prevent Fitness Decline
- Sedentary people had much different trajectories.

According to a new study published in Aging Cell, previously sedentary old people who took up an exercise program were able to improve their fitness and maintain it for at least four years [1].
Better late than never
When is it too late to engage in physical activity? The answer might be “never”. Physical activity is one of the most potent anti-aging interventions currently available. When done properly, it can slow numerous aging processes and vastly increase life quality [2]. However, many older people behave as if it is too late for them to take up exercise and enjoy its benefits. While research suggests that this is not the case [3], there is a lack of studies with long-term follow-up.
A new study cleverly employs two different cohorts to fill this gap. One of the cohorts comes from Gerofit, a US study in which previously sedentary elderly people (mean age 72.5) were enrolled in a six-month age-appropriate exercise program. The new study included 318 people who stuck to the exercise program past the six-month mark and were followed up with once a year for four years.
The second cohort of 146 people (mean age 74.5) was taken from the Italian study Act on Aging (AOA). Those individuals had self-reported leading sedentary lives for the last five years prior to their enrollment in the study and remained sedentary for one year, when their fitness was measured again. The researchers essentially used the AOA cohort as a control group for the Gerofit cohort, due to the relative similarity of characteristics at baseline in both cohorts.
Long-term fitness retention
Fitness levels were measured using three popular metrics: the six-minute walk test, in which distance is measured; the 30-second chair stand, which measures the number of times a person can get up from a chair and sit back down; and, finally, the up-and-go test. The latter measures the time a person needs to stand up from a chair, walk three meters, turn around, walk back to the chair, and sit down.
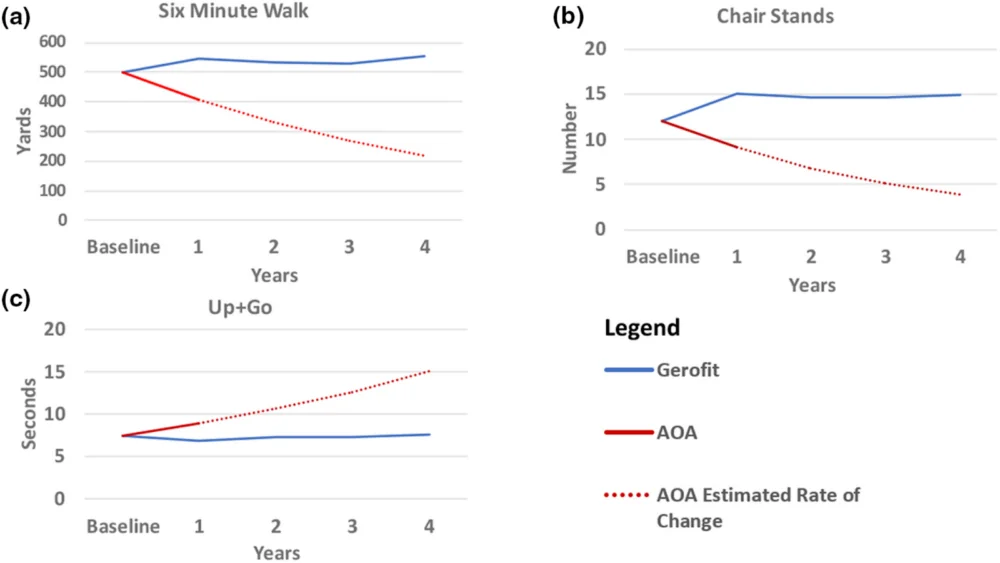
During the first year, the Gerofit cohort showed noticeable improvement in all metrics, while the AOA cohort suffered an even more drastic decline.
In the six-minute walk test, the Gerofit cohort improved distance by 44.1 yards (10.9%), while the AOA cohort’s average distance declined by 75.8 yards (−18.7%). In the 30-second chair stand, the Gerofit cohort showed an improvement of 3.1 (30.6%). The AOA cohort’s numbers declined by an average of 3.2 chair stands (−24.5%). In up-and-go tests, the Gerofit cohort improved their time by 9.2%, while the AOA cohort’s performance at year’s end plummeted by 19.4%.
While Gerofit cohort’s numbers did not improve after the first year, they did not decline either, showing strong resistance to age-related changes that sharply affected the AOA cohort’s performance. Since there was no follow-up for the latter cohort past the one-year mark, it is possible that the rate of decline attenuated during the following years. Lacking this information, the researchers simply extrapolated the first year’s results.
Survival of the oldest?
The researchers also divided the cohorts into three subgroups by age, 65-74, 75-85, and 85+, to analyze their respective trajectories.
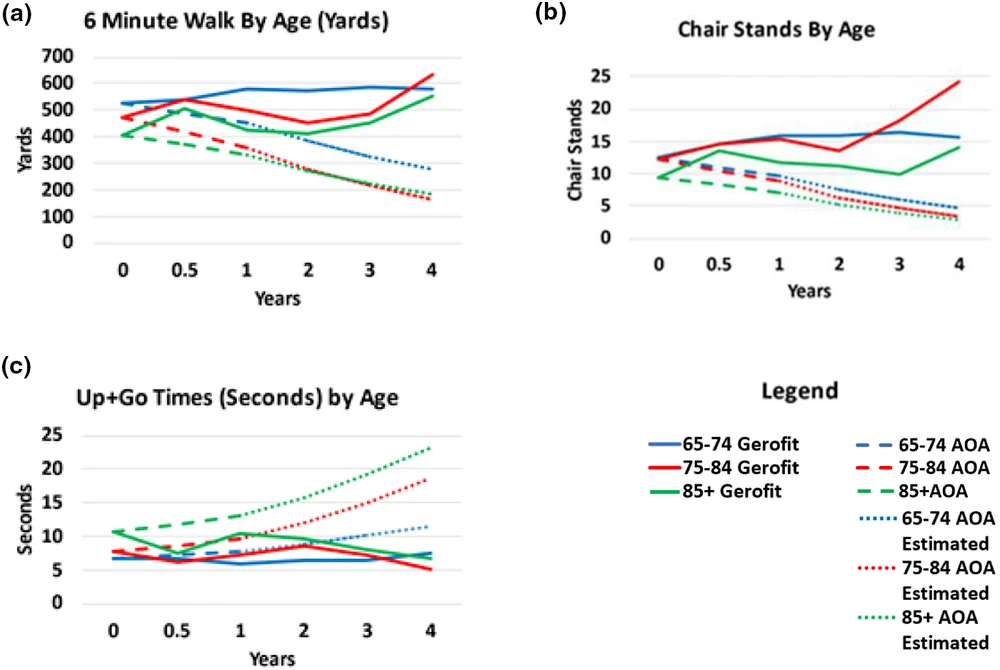
In the AOA cohort, all subgroups suffered a similar decline in their physical abilities, but in the Gerofit cohort, the analysis produced some unexpected results. In the six-minute walk test, the three subgroups differed at baseline, but at the end of year 4, they showed almost identical results, with the 75-84 subgroup slightly outperforming their younger counterparts. In the chair stand test, the 75-84 subgroup’s surge was even more evident. However entertaining, those results should be taken with a grain of salt, since dividing into subgroups lowered the study’s statistical power.
The main upshot is deeply optimistic: despite being pretty much couch potatoes at baseline, the Gerofit participants were able to substantially increase their fitness during the first year, overpowering the deleterious effects of aging evident in the second cohort. Moreover, they managed to stay fit for a considerable period of time late in life.
The study also suffered from several limitations. First, while the differences at baseline were moderate, some of them may still have affected the results. Importantly, both cohorts were overweight (mean BMI of 30.6 for Gerofit and 26.9 for AOA), which raises questions about the generalizability of the results. Second, using a completely different cohort as a control group is less than ideal. Finally, both cohorts were almost exclusively male, which can pose a problem due to the well-known gender differences in aging trajectories. Hopefully, we will see more robust studies with proper randomization, larger sample sizes, and an even gender distribution that confirm this one’s findings.
Literature
[1] Manning, K. M., Hall, K. S., Sloane, R., Magistro, D., Rabaglietti, E., Lee, C. C., Castle, S., Kopp, T., Giffuni, J., Katzel, L., McDonald, M., Miyamoto, M., Pearson, M., Jennings, S. C., Bettger, J. P., & Morey, M. C. Longitudinal analysis of physical function in older adults: The effects of physical inactivity and exercise training. Aging Cell, e13987.
[2] Harridge, S. D., & Lazarus, N. R. (2017). Physical activity, aging, and physiological function. Physiology, 32(2), 152-161.
[3] Berk, D. R., Hubert, H. B., & Fries, J. F. (2006). Associations of changes in exercise level with subsequent disability among seniors: a 16-year longitudinal study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 61(1), 97-102.