iPSC-derived Cardiomyocytes Rescue Heart Damage in Monkeys
- The grafts offered imperfect but significant improvements.

Scientists have successfully used heart muscle cells created from induced pluripotent stem cells to counter the deleterious effects of heart attack in non-human primates.
Reprogrammed cells for heart regeneration

Read More
Since Dr. Yamanaka’s discovery, there has been a massive effort to turn this discovery into working therapies, with some of those experimental treatments currently nearing fruition. For instances, induced pluripotent stem cells (iPSCs) can be differentiated again into various types of youthful functioning cells.
Scientists have tried for a while to utilize iPSC-derived heart muscle cells (cardiomyocytes), to treat the consequences of myocardial infarction (heart attack) [1]. Healing after a heart attack is imperfect: stiff fibrotic scar tissue forms where healthy muscle was, leading to impaired heart function. However, attempts to infuse the healing muscle with iPSC-derived cardiomyocytes have been hampered by poor engraftment and posttransplant arrythmias, the latter caused by significant differences between the electrical qualities of adult cardiomyocytes and iPSC-derived ones.
Furthermore, before such problems can arise, most injected cardiomyocytes are thought to be simply washed away by circulating blood. Even those that remain are subject to a special type of cellular death, anoikis, caused by poor attachment to the extracellular matrix.
Spheroids instead of single cells
The Japanese researchers who authored this new study had learned about all these problems the hard way, from the results of their previous studies. This time, they decided to do things differently. In this new study performed on non-human primates (cynomolgus monkeys), which are far better models than rodents, instead of inoculating the monkeys with “free-floating” iPSC-derived cardiomyocytes, the researchers used spheroids: tiny balls of cells that form after several divisions. The researchers hoped that this would lead to better survival, engraftment, and integration of the cells into the existing electrical network of the heart muscle.
After receiving frozen human iPSCs from Kyoto University, the researchers differentiated them into cardiomyocytes. The cells were then frozen again for transportation to the animal lab and thawed without hurting their viability. The freezing-thawing part, according to the authors, is important because it shows suitability for future clinical use. Having grown the spheroids, the scientists injected them into 10 monkeys who had undergone heart attacks.
Partial rescue of heart damage
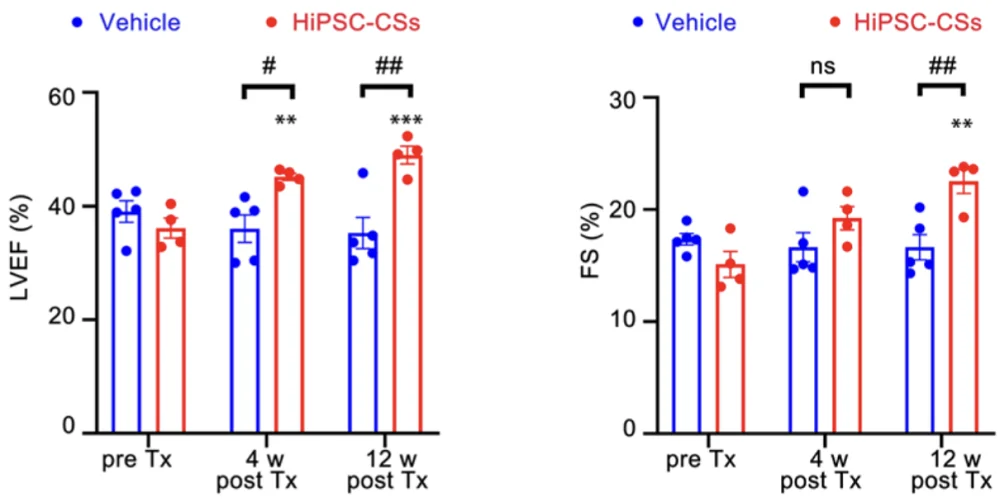
At first, the dose used was 20 million cells. Four weeks after transplantation, the heart contractile function of the treated monkeys was significantly improved versus controls, but the difference fell below the level of statistical significance at the 12-week mark, despite the difference between the 4-week and the 12-week readings being minuscule.
Since the resulting grafts were small, the researchers decided to increase the dose. Another ten monkeys were inoculated with 60 million cells each. This led to much better engraftment and to sustained (albeit only slightly bigger) benefits in cardiac function. Moreover, the improvement at the 12-week mark was more significant than at the 4-week mark. On the other hand, comparing cardiac function of the treated monkeys to that of healthy ones suggested that the treatment had only resulted in partial restoration.
Despite the greater number of transplanted cells, none of them were detected in other tissues such as lungs, suggesting highly targeted engraftment. The graft cells’ maturation levels were close to those of the host cells, and the graft was adequately supplied by blood vessels. Unfortunately, the larger dose also caused more arrythmias, but those symptoms were mild and short-lived. The researchers did not detect “any apparent immune response”, which is an encouraging result even though the monkeys were immunosuppressed.
According to the researchers, cardiac spheroids “have several advantages and may be an ideal form of a cardiomyocyte product for cardiac regenerative therapy”. For instance, they proved to be more viable than single cells, surviving for at least four hours at 4°C (39°F), which significantly improves transportability.
Literature
[1] Wu, P., Deng, G., Sai, X., Guo, H., Huang, H., & Zhu, P. (2021). Maturation strategies and limitations of induced pluripotent stem cell-derived cardiomyocytes. Bioscience Reports, 41(6), BSR20200833.