Genetically Enhancing T Cells to Fight Tumors
- These cells might be far more effective than current immunotherapies.

A team of researchers from multiple Japanese universities has found a way to genetically enhance T cells against solid tumors, as published today in Nature Biomedical Engineering.
A focus on signals
This highly in-depth paper begins with a discussion of signaling in the response of chimeric antigen receptor (CAR) T cells, as good signals are vital for their effectiveness [1]. Three specific biochemical signals are mentioned: a primary signal that spurs the downstream activation of T cells, a co-stimulatory signal that sits on the surface of T cells to enhance the primary signal, and a cytokine signal that promotes the activity and survival of T cells.

Read More
Previous work has dedifferentiated T cells into induced pluripotent stem cells (iPSCs), which then redifferentiate back into rejuvenated T cells [2]. However, these cells have been imperfect, particularly with regards to signaling. One experiment used added signals to enhance the effectiveness of such cells [3], but these researchers note that this approach is much stronger against blood-borne cancers than solid tumors.
Thorough enhancement
Seeking to improve cellular signaling from the inside out, the researchers performed three modifications to their cells. The first was to select a CAR differentiation line that did not send exhaustion signals, promoting the formation of T cells. For the second, the researchers used the well-known CRISPR/Cas-9 technique to inhibit the cells’ response to counteracting signals that might be found within the tumor. For their final modification, the team enhanced the production of the cytokine IL-15.
The researchers tested their modifications every step of the way. The first modification, applying this CAR to these T cells, made the cells much more effective than similar cells without it, but this modification could also be applied to primary T cells, which were much more robust and effective than these iPSC cells.
The second modification improved the cells further. The cells’ metabolic fitness was improved, they survived for longer, and they fought tumors more effectively. Simply put, they became better at being T cells. These genetically modified cells were nearly as effective against solid tumors as the primary CAR-T cells.
The third modification changed the game.
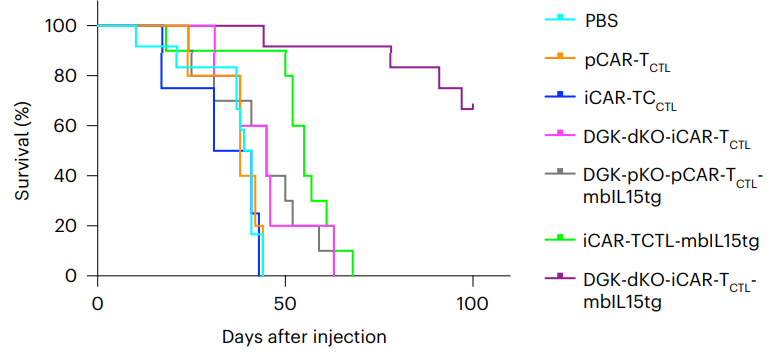
While this suite of modifications could not be effectively applied to primary T cells, the iPSCs took it very well, significantly outperforming the other groups in every respect and dramatically improving survival against a model of ovarian cancer. Further testing showed that it was nearly as effective against a model of liver cancer. Tumors, while they still grew somewhat, were much slower to grow when these triply modified cells were present.
Conclusion
While proven to work only in mice, this approach represents a significant breakthrough for immunotherapy. It is easy to envision that this team, or other teams, may discover even more alterations that improve iPSC-derived T cells even further against cancer. Because these modifications begin with a single cloned cell, they can be applied with 100% accuracy, sidestepping a problem common to gene therapy.
However, as the researchers note, this approach is not without its potential drawbacks. The modifications to these cells primarily worked by making them considerably more aggressive, which might enhance negative immune reactions in human trials. This paper recommends suicide genes and other modifications to prevent immunorejection and make such cells safe for general use against cancerous tumors in human beings.
Literature
[1] Klebanoff, C. A., Gattinoni, L., Palmer, D. C., Muranski, P., Ji, Y., Hinrichs, C. S., … & Restifo, N. P. (2011). Determinants of Successful CD8+ T-Cell Adoptive Immunotherapy for Large Established Tumors in Mice. Clinical Cancer Research, 17(16), 5343-5352.
[2] Nishimura, T., Kaneko, S., Kawana-Tachikawa, A., Tajima, Y., Goto, H., Zhu, D., … & Nakauchi, H. (2013). Generation of rejuvenated antigen-specific T cells by reprogramming to pluripotency and redifferentiation. Cell stem cell, 12(1), 114-126.
[3] Iriguchi, S., Yasui, Y., Kawai, Y., Arima, S., Kunitomo, M., Sato, T., … & Kaneko, S. (2021). A clinically applicable and scalable method to regenerate T-cells from iPSCs for off-the-shelf T-cell immunotherapy. Nature communications, 12(1), 1-15.







