Lou Hawthorne, NaNotics on Cleaning Blood with Nanoparticles
- Removing inflammatory cytokines may be key to fighting many diseases.

Lou Hawthorne is the founder and CEO of NaNotics, a biotech company that creates nanoparticles that can soak up harmful molecules in circulation. This paradigm-shifting technology can be used to fight cancer as well as various inflammatory disorders, such as sepsis, which kills more people than cancer does. Other potential targets, familiar to everyone in the longevity field, are age-related sterile inflammation (inflammaging) and cellular senescence. Amazingly, Lou is an autodidact who earned his place in the field with his ingenuity and relentless pursuit of knowledge.
What is your story? What was your journey to the longevity field?
Before I got into science almost 30 years ago, I was a professional graphic designer, cinematographer, and editor, mostly in the Bay Area. In addition to creative work for various clients, I also consulted on highly technical feasibility studies on the integration of digital media and broadcast video, which in the 1980s and early 90s involved a number of challenges that no longer exist.
I got drawn into science through a documentary I worked on for a couple of years about the Biosphere 2 project in Arizona, a self-contained biological habitat. Making a documentary involves such an enormous amount of time and effort that you naturally become an expert in the subject matter, so this documentary was a crash course in botany, animal physiology, atmospheric geology, and many other scientific topics. That was my first very deep dive into science aside from an immunology course in college. I surprised myself not just with how much I loved the scientific side of this project but also by my facility at absorbing the material.
Not long after Dolly the sheep was cloned, I was hired to explore the feasibility of cloning the pet dog of a billionaire. I had no particular knowledge of cloning, but I had some basic scientific knowledge and I knew how to organize a feasibility study. I wasn’t a bad choice for this role; there wasn’t anyone in particular you could call at the time to clone your dog!
I was originally hired to do a three-month feasibility study on dog cloning. After speaking to various experts – including at Roslin Institute in Scotland, where Dolly was cloned – I delivered a report to my client stating that just because sheep had been cloned, that didn’t mean dogs could be cloned, given that their reproductive physiology was quite different. Even assuming dogs could be cloned, it would require years of very expensive work. I figured that delivering this report would be the end of my involvement, but much to my surprise I was hired to perform the next step: assembling a team of experts capable of completing the work.
Over the next several years, I became something of a cloning expert. That was my first real domain of expertise in science. Cloning is very much about cellular signaling, given that the embryo is in constant molecular communication both with itself and with the surrogate that carries it. Much of this communication is immunologic. The surrogate’s immune system is naturally on guard against foreign invaders of all types. When you insert a cloned embryo into the recipient’s uterus, the goal is to create immunologic “privilege” – meaning the surrogate’s immune system allows the cloned embryo to persist and grow inside her, despite being genetically unrelated to her. All pregnancies – even with non-cloned embryos – actually face a similar problem, given that an embryo produced sexually is only half the mother and thus should be destroyed by her immune system as a parasite.
I became very interested in the molecular mechanisms of immune privilege – how they work and why they sometimes don’t work.
Along the way, I would often hear cloning scientists speculate that the insights we were gaining in cloning might someday lead to cures for cancer. I gradually began to realize that cloning animals and treating cancer are actually mirror processes from an immunologic standpoint. When you clone, you’re trying to create immunologic privilege: to trick the recipient’s immune system into tolerating a foreign embryo. Cancer cells are also abnormal, yet the immune systems of cancer patients tolerate their tumors, because tumors create the same type of immune privilege that a successful embryo creates. When you treat cancer, you’re not trying to create immune privilege as you are with cloning; you’re trying to strip it away.
I ended up spending more than a decade founding and leading various companies developing cloning technology for multiple species: cat, dog, horse, and cattle. The world’s first clone pet dog was actually a clone of my mom’s dog. She became my beloved companion.
Wait, you actually had a clone dog as a pet?
Yes, for twelve and a half years till she died of old age, just a couple of years ago. Her name was Mira. She was an absolute sweetheart. I adored her. Mira was a clone of my mom’s dog Missy. We made four clones of Missy (we referred to them as the “near Missies”). Mira was the first born.
I just have to ask: did they differ in character, in personality?
The clones were of course physically identical, or as close to that as identical twins. They all started out with very similar behavioral tendencies because part of what gets cloned is the brain, so their neurological wiring was very similar. They responded to various stimuli in very similar ways; for instance, how they reacted to sounds. When they ran, they would run like a flock of birds. They would stop at the same moment, turn their heads at the same moment. They were all very curious and very good with language, picking up new words very quickly. They didn’t necessarily obey commands, because another similarity they had with each other and their genetic donor is that they were all very strong-willed. But they definitely understood what their humans were saying.
As they got older, their personalities started to diverge from each other and the “original” Missy (who had died years before they were born). The Missy clones were raised by different people with different lifestyles, which accelerated their divergence.
I was raising my son Skye at the same time. He had known the original, Missy, as a toddler, and he grew up surrounded by clones of her. It was a wonderful experience for all of us, a nature-vs-nurture experiment in our own home.
Along the way, I continued to study science, gradually moving beyond embryology but with a consistent interest in cellular signaling, which seemed to connect biology to information science, which I had been exposed to in my prior career in digital media.
I shifted my whole focus to disease and aging, with a particular emphasis on the role of pathogenic cell signals and signal inhibitors. The history of medicine began by focusing on organs, which you can easily see with the naked eye, then tissue, then cells. We’ve been able to see cells for 300 years since the invention of the microscope, and this has led to almost a fetish for cells as the locus of disease.
Over the last few decades, we’ve started to be able to detect what’s going on at scales below that of the cell, including the molecular signals that pass between cells, especially cytokines, the signaling molecules of the immune system. Once you investigate these intercellular signals, you realize that they play just as big a role if not bigger than any pathology that happens inside a cell.
In 2008, a dear friend of mine, one of my mentors in cellular signaling, a PhD endocrinologist named Chris Heward, developed stage 4 metastatic esophageal cancer. My investor was also his investor in a company called Kronos, which was focused on human longevity. I believe Kronos was the first really well-capitalized longevity research company, formed around 2000. They were focused on both age-related diseases and mechanisms of aging and published some important findings.
We all loved Chris. He was brilliant, funny, and outrageous. Our investor gave us a blank check “to find something that would save Chris.” That was how I came across a technology in Germany called Immune Pheresis, which treats cancer by depleting tumor-generated immune inhibitors from blood, using apheresis, an extracorporeal method of filtering blood, basically a more advanced version of dialysis.
The specific molecules that Immune Pheresis was depleting were soluble tumor necrosis factor (TNF) receptors. TNF is the body’s main “death signal”, normally delivered by immune cells directly to abnormal cells. TNF instructs an abnormal cell to commit suicide, a process called apoptosis. To protect themselves against TNF, cancer cells, like the human placenta, cleave off the extracellular portion of the TNF receptor, so it’s no longer connected to a cell. This extracellular receptor portion is then called an sTNF-R, the “s” meaning “soluble”, i.e. dissolved in blood. sTNF-Rs intercept and neutralize incoming TNF before it can reach a target cell and induce apoptosis.
We were too late to save Chris, who died just three months after his diagnosis. We were all just devastated.
However, we witnessed some phenomenal regressions induced by Immune Pheresis in patients who had already failed standard of care, meaning no improvement by any means would be expected. About 60% of the patients undergoing this treatment had significant regression of disease, including a surprising number of complete remissions. Even after Chris died, our investor encouraged me to dig more deeply into this data. Further studies confirmed that Immune Pheresis worked, that you could get regression and sometimes even full remission just by taking something out of their blood without adding anything at all.
We wanted to learn more about these inhibitors. We confirmed that the Immune Pheresis device can routinely deplete them by about 70% (NaNots can deplete them by 95%) over a 3- to 4-hour treatment. This alone could make the difference between tumor progression and regression in a patient with multiple kilograms of tumor. We measured the aggregate mass of the sTNF-Rs being depleted in a single treatment, which turned out to be 10 to 12 micrograms. That’s it. By depleting this minute amount of inhibitors, you tilt the battle in cancer away from the tumor and toward the immune system, ultimately leading to regression. You have to repeat the process several times, but it’s still a phenomenal result, entirely without drugs and the associated toxicity.
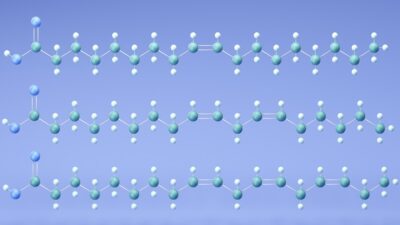
A profound question came out of these studies: Why do you need a refrigerator-sized device just to deplete 12 millionths of a gram of immune inhibitors from blood? Surely we could design something injectable that would do the same thing? This question triggered the creative process that ultimately led to the invention of NaNots.
This is a fantastic story, and I am sorry about your friend and mentor. So, you accomplished all of this without formal training in biology?
That’s correct. I’ve been interested in science and science fiction since I was a child, but I have no scientific training other than what I picked up working with scientists in various companies and on projects I was managing. In some ways it’s harder to be an autodidact. You have no laurels to rest upon, so you have to be constantly learning and innovating in order to be taken seriously.
Actually, at the end of the day, everyone is an autodidact because no one can just pour knowledge into your brain. You have to learn it yourself. I learn the same way any PhD learns. I read books and scientific papers, I go to conferences, and I get mentored one-on-one by experts in the field.
There are two key differences in my approach to learning science versus that of the average PhD. One, I wrote my own syllabus. For better or worse, no department head told me what I needed to study. Two, nobody has validated my knowledge in a formal way with a certificate or a degree. My validation comes through invention: the technologies I’ve designed and patented that actually work. There’s no arguing with that.
This should be really inspiring for many people.
I hope so. There’s a new generation of serious biotech scientists who are autodidacts or come from fields other than biology, such as Matthew Scholtz, who runs Oisin. He came from computer science, not biology, but he’s become a fantastic and highly innovative biological thinker. There are more and more like us. Traditional academic educational pathways that train you to think in certain ways aren’t necessarily the best pathways for developing truly orthogonal therapeutics; they certainly aren’t the only pathways. Interdisciplinary backgrounds can be very helpful for conceptualizing novel solutions.
Let’s dig deeper into NaNotics’ technology. Could you start by briefly explaining the concept?
First, it’s important to understand the challenge we were aiming to overcome. When I asked the inventor of Immune Pheresis whether there was something that could be injected into the patient that would do the same thing as his pheresis technology, he gave me a brilliant two-hour lecture over dinner on why that wasn’t possible.
His main point – and I’m oversimplifying a bit here – was that if you target soluble TNF receptors with a drug, that drug is also going to bind and block membrane TNF receptors, because they’re biochemically identical. But membrane TNF receptors are a pathway that must be kept open, because innate immunity in particular depends on it. So, a drug against soluble TNF receptors would wreck innate immunity, and patients would die very quickly.
This challenge didn’t seem insurmountable. It made sense that you couldn’t achieve the goal with an antibody drug, but the micron-scale engineering I had overseen as part of my cloning work made me wonder if it might be possible to create an engineered structure at the nano scale that could capture the soluble target form (sTNF-Rs) without disturbing the membrane form (TNF-Rs), despite the fact that they’re biochemically identical.
The “eureka moment” came while hanging out with my cloned dog Mira. At the time, she had a minor skin infection and was wearing that cone that they put on dogs’ heads. I was feeding her a treat through the cone, and noticed that although the cone prevented her from biting her skin, she could still take treats from my hand. At that moment, I realized we could design a nanoparticle covered with capture agents with a little cone – or something like a cone – over each of them. They could still capture soluble factors, but the cone would prevent contact between the capture agents and cellular surface proteins of all types, including TNF-Rs.
Then it became a question of “How do we design that?” I did a bunch of sketches, and I started passing them around to scientists and nano-engineers that I knew. We also searched the scientific literature and patent records for something similar – nothing. Nobody had ever done it, which amazed me. Then I started talking to prospective investors. Among them was Jonathan Milner, founder of Abcam, the world’s largest public company focused on antibodies, and he became our first seed investor. Our next step was mathematical in silico modeling of various particle designs.
I thought it would probably take about as long for our nanoparticles to absorb their targets as pheresis – three to four hours. But the math showed that our nanoparticles would start working within seconds. Even with a very low aggregate mass of particles (we currently project one to two milligrams per kilogram, of which 95% is inert silica), that mass is distributed across trillions of particles. That means that within a few heartbeats, our typical nanoparticle and the typical target would be less than a micron apart, and diffusion driven by Brownian motion would bring them together within seconds.
Along the way, we named the particles “NaNots”. The inclusion of “Not” within the name is important, because NaNots are the opposite of a drug; they deplete their targets rather than adding molecules. NaNots can reverse a large number of biological processes by depleting either a pathogenic signal or an inhibitor of a healthy signal.
I find information science to be helpful in understanding biology. I view cells as basically little computers. With computers, the output they send depends to some extent on the inputs they receive. The same is true with cells. A cell’s “ROM” or prewritten code is the gene sequence. This coding includes many branching responses depending on signals picked up by cell surface receptors, which lead to changes in epigenetics. Cellular function can change dramatically based on signals received from outside the cell. The cell may die, or proliferate, or do any number of other things, and incoming signals also may change the signals that the cell sends out.
In the early days of computer science, we were very focused on the computer itself and on the software that you load into it. Nowadays, the computer is basically irrelevant, it’s just a portal to information in the cloud. A similar shift is happening in biology. We still pretty much fetishize the cell and its internal workings, but it’s becoming more apparent that cells largely do what they’re told based on signals they receive from other cells. This is true in both health and disease. You can have a disease manifest itself at a tissue or organ level, but when you investigate what’s happening at the cellular level, you often find that cells are doing exactly what they’re supposed to be doing relative to the signals they’re receiving. It’s the signals that are wrong or don’t reach their intended target.
One can even make a credible argument that in terms of health and disease, the network of cell signals is what really matters; cells themselves are just logic gates and depots of materials needed to maintain that network.
I guess not for nothing altered cellular communication is one of the hallmarks of aging.
Definitely. However, this wasn’t one of the original hallmarks. It was added because people like me were insisting that we mustn’t forget about the role of aberrant intercellular communication in disease and aging. Some of us believe this dysregulated signaling between cells is really most of the game of age-related diseases and aging itself. It’s certainly a huge part.
We now understand that tumors, like the fetus/placenta, defend themselves with immune inhibitors, both membrane and soluble inhibitors. It’s more than an analogy, because tumors and the fetus/placenta use the same molecules to inhibit immune attack. The inhibitors used by embryos and tumors are also employed by senescent cells, which makes sense because senescent cells are halfway to cancer when P53 suppresses them.
This last idea, that senescent cells defend themselves with soluble immune inhibitors, is still new and controversial. I’m one of the few scientists that’s arguing this point. The senescence-associated secretory phenotype (SASP) produced by senescent cells is packed full of immune inhibitors. What are they doing in the SASP if not protecting senescent cells from immune-mediated destruction? It takes a lot of cellular resources to produce these inhibitors, and cells don’t do that for no reason.
When most scientists think about immune inhibition – or cellular signaling at all – they gravitate toward membrane signaling. This is a natural tendency because membrane signals are on cells, and we tend to fetishize cells, as I mentioned. Checkpoint inhibitors in cancer were developed based on this idea that cells control each other through membrane interactions.
Let me use a military analogy here. The soldier only wants to use his bayonet as a last resort when the enemy is right on top of him. Prior to that, soldiers prefer to use bullets, to kill the enemy at the greatest possible distance. In the body, the fetus, the tumor, and senescent cells all use soluble immune inhibitors to inhibit the immune system at a distance, before they rely on membrane immune inhibitors in a last-ditch attempt to defend themselves from immune-mediated destruction.
I understand that NaNots are cleared by macrophages, right? How does this happen, and how safe in general NaNots are?
NaNots are particles, and particles are naturally cleared by macrophages. Any foreign particle is going to be phagocytized by macrophages. This would normally happen within minutes, but we can delay it for up to about 16 hours by attaching a “stealth” coating to the NaNots.
This coating prevents opsonization, which is the attachment of protein markers that flag a particle for clearance by macrophages. Eventually, NaNots get engulfed by macrophages and broken down – along with their cargo of captured proteins – into small molecules, which are then excreted.
The current generation of NaNots are built on a core of silica, which has been used in other nanomedicines and is well-known for its ultra-low toxicity (if properly coated). Although no one’s ever made a NaNot before, the same materials are used in other nanomedicines that possess a very good safety profile, both at the macro “whole animal” level and in terms of macrophages.
We’ve dosed NaNots in rodents at 100x the planned dose in humans, and we haven’t seen any toxicity yet. None. Based on our data so far, we believe NaNots are completely non-toxic, which is unheard of for a drug, especially a drug against a major disease like cancer or sepsis. We haven’t talked about sepsis yet.
Let’s do it. The applications seem to be infinite because we’re talking about molecules in the circulation and intercellular communication, so I understand that it can be used against sepsis, autoimmune diseases, and even cellular senescence?
Any time you have a new therapeutic strategy, usually it ties into a whole ontology of disease that might be different from regular disease ontologies. For instance, with checkpoint inhibitors, now all of a sudden tumors are being classified as “hot” versus “cold” in terms of how immunogenic they are. That’s new.
In our ontology, there are three kinds of disease: There are genetic diseases, which we don’t touch; they actually only account for less than 10% of all diseases. The vast majority of other diseases are either inflammatory, driven by an inflammatory cytokine or cytokines, or inhibitory diseases where you have aberrant cells defending themselves with immune inhibitors.
Sepsis is the most acute form of inflammatory disease, in which the immune system massively overreacts to a trigger of some kind. Some people confuse sepsis with infection, but infection is just one of several possible triggers of sepsis. The morbidity and mortality of sepsis is due to the immune system’s overreaction, not the trigger.
It’s a kind of cytokine storm, right?
Correct. A cytokine storm is a positive feed-forward loop, stemming from the fact that cytokines are pleiotropic, meaning they have multiple effects. When TNF lands on a non-immune cell and ligates the TNF-R1 receptor, it induces apoptosis, which destroys the cell. When TNF is received by an immune cell and ligates the R2 receptor – which is preferentially expressed on immune cells – it induces proliferation and activation of that immune cell.
Under certain circumstances, the initial cytotoxic immune response supported by TNF-mediated recruitment of additional immune effector cells can spiral out of control. It’s analogous to a nuclear meltdown following the failure of a reactor’s cooling system. Once the meltdown starts, you can spray all the water you want on the reactor, and it won’t stop the meltdown.
The pleiotropy of TNF is an evolved mechanism of enhanced immune response, and normally it works really well, with the occasional biological “cost” of sepsis. TNF pleiotropy offers a net benefit in terms of the survival of the species even though the cost at a population level is quite high: sepsis kills more people than all forms of cancer combined.
Clinicians like to emphasize that sepsis is very complex. We view it a little differently. Wherever the cytotoxic cytokines involved in sepsis touch tissue, that will result in a clinical complication. Given the broad array of tissues that can be hit by these systemically elevated cytokines, you can incur a broad range of clinical complications, but the base driver of the storm is not complex. It’s mainly driven by three inflammatory cytokines released in a cascade: TNF-α, which is the upstream driver of the cascade, followed by IL-1ß and IL-6. There are other cytokines involved, but those are the main players.
TNF is the first responder, IL-1ß organizes a coherent immune response (or over-response), and IL-6 is more generally a “soldier” that inflicts most of the damage. If you soak up those molecules, the clinical complexities don’t arise and thus don’t matter. You can extinguish the storm. You’ll have to deal with the damage that’s already been incurred, but you can stop the runaway reaction and prevent further damage and death. It’s like pushing the control rods back into the reactor before the meltdown occurs. That’s what anti-inflammatory NaNots will do. They’ll soak their target cytokines rapidly and thoroughly before the process spirals out of control.
There are drugs against all those cytokines, but they don’t work in cytokine storm for several reasons. First, they’re not specific to soluble cytokines. They also hit the membrane form of TNF (for instance) stored on the surface of immune cells. If you administer an anti-TNF drug, you’re going to neutralize membrane TNF on the surface of immune cells in addition to the targeted soluble form, and there goes your immune competence. You can’t do that in sepsis because you often still have an active pathogen that triggered the sepsis in the first place. Treating sepsis requires that you neutralize the systemically elevated cytokines without reducing immune competence. That’s the part no one has ever cracked.
The second reason why those drugs don’t work is that their arc – their persistence in circulation – is too long. They last for days in the blood, which aggravates a later stage of sepsis known as “immune paralysis”. Many patients die in this phase, when the body throws every immune inhibitor it has against the cytokine storm. Anti-inflammatory drugs that last for days drive the patient deeper into immune paralysis, whereupon they die of whatever nosocomial infections are floating around the hospital. The effect would be like HIV.
So, the DMARD drugs against cytokines are the wrong tool. You want something that only hits the soluble form, doesn’t disturb the membrane form, and only acts in circulation, without extravasating into tissue. Finally, you need something that acts fast and clears rapidly. These parameters describe NaNots perfectly.
But that means that after an initial injection, the levels of cytokines that you’re trying to deplete are going to go back up. So, how does the delivery work – do you need multiple injections or, maybe, continuous intravenous delivery?
They may go back up, or they may not. What we know for certain is that the first injection of NaNots will deplete the target to near zero. With this, you achieve two things at once. First, you interrupt MODS – multiple organ dysfunction syndrome, the main killer in sepsis. That’s when organs start to fail, which happens for two reasons.
One, blood pressure crashes, because part of those cytokines’ natural purpose when expressed at low levels during infection is to increase the permeability of the vasculature so that immune cells can get to pathogenic cell clusters faster. When expressed at very high levels in sepsis, you get leaky vasculature, blood pressure drops, then the organs don’t get enough blood and begin to die. Of course, the cytokines also directly attack the organs as well. Both of those processes will be abrogated by soaking up the cytokines with NaNots.
However, even assuming you fully deplete the cytokines that were recruiting immune cells, it’s possible that some of those immune cells are now dysregulated and will persist in a hyperstimulated state, cranking out excess inflammatory cytokines systemically, even after the first dose of NaNots. So, it’s possible that after soaking up all the inflammatory cytokines initially, you may need to administer another dose of NaNots to address subsequent release.
But with each dose, you’re stopping the tissue damage stemming both from apoptosis of cells in organ tissue and from permeation of the vasculature, and you’re eventually breaking the storm. Patients usually die of sepsis in five to seven days. Even if you have to inject the patient half a dozen times during that period, that shouldn’t be an issue given the ultra-low toxicity of NaNots. You just monitor the patients, measure their cytokines before, during, and after treatment, and administer the specific NaNots needed in the doses required.
I can understand how it can work in a hospital environment, but how can it potentially be used against inflammaging, as a preemptive anti-aging treatment?
That’s a good question. Not everybody accepts it, but I think there’s a consensus that inflammaging is real and that it’s a driver of not just age-related diseases but of aging itself. Inflammation is a critical target for anti-aging therapy.
I personally think that, if anything, inflammation is probably underappreciated as a driver of age-related diseases.
I would agree. Anyway, it’s clearly a real thing. We know that because these cytokines rise with age. In healthy young people, they’re at or below the level of detection. There’s no purpose served by them being elevated systemically. If they are constantly elevated, which we see in older people, it’s like the difference between a sniper taking out a terrorist with a precise kill shot, versus a madman spraying bullets in every direction. Sorry for all the military analogies, but I really feel like there is a war going on in the body.
In order to treat Inflammaging, we have to soak up these excess inflammatory cytokines not just over a period of days as in sepsis but over a period of decades. Our current GEN-2 NaNots circulate for 16 hours, which is great for treating acute conditions, but if you want to treat somebody, say, once a week for decades, you need an ultra-low toxicity, non-accumulating technology, and that’s not silica. When treating serious diseases over weeks or months, our GEN-2 NaNots are non-toxic – certainly compared with checkpoint inhibitors, chemotherapy, et cetera – but they’re not zero toxicity.
So, for treating aging, we’re developing GEN-3 NaNots, which are polymer-based. You should be able to dose somebody with GEN-3 NaNots every week for the rest of their lives with no cumulative negative effects. In our vision of NaNots used as a longevity treatment, you’ll swing by your local Quest for a measurement of the signals and inhibitors that are elevated in your body, then you’ll receive an injection of just the right NaNots in the right dose to bring your intercellular communication into balance. We already have a slogan for that service: “Get Your Signals Straight!”
I think this is the future of anti-aging therapies: everyone will be getting a weekly or a monthly appointment, with several therapies thrown at them for the rest of their lives.
Why not? Interestingly, I’ve had several cycles of therapeutic plasma exchange, and it feels amazing when you get these inflammatory cytokines cleared from your blood. You feel it immediately. I suspect that NaNots will feel amazing too. Inflammatory cytokines rise steadily with age, they degrade tissue and organs throughout your body, and they easily cross the blood-brain barrier and drag down your cognitive function too. So, once you clear them out or reduce their concentration, you are going to feel it.
Because this is such a universal technology, the list of potential targets can go on and on. Can you briefly tell me about your current pipeline?
We have a pipeline of eight NaNots (with dozens more in line after that). Four of them are against the inflammatory cytokines that drive many canonical inflammatory diseases like arthritis and psoriasis along with the newly understood non-canonical autoimmune diseases like type 2 diabetes and atherosclerosis. For instance, the calcification that happens in atherosclerosis is driven by TNF.
PTSD, depression, all sorts of cognitive disorders, cardiovascular diseases – these are cytokine disorders as well. Pro-inflammatory cytokines rise with age, and whatever they touch has a protective response against it. Heart cells calcify. Why do they do that? Because they can’t be allowed to die, so they do something that isn’t ideal: they calcify instead, which is a known response to excess circulating TNF.
Likewise, when the brain is exposed to inflammatory cytokines, it forms plaques. That’s not ideal either, but from an evolutionary perspective, it’s better than the brain dying. Many processes that happen in the body are basically suboptimal protective responses against these inflammatory cytokines. We’re focused on “the big four”: TNFa, IL-1ß, IL-6, and IFN-γ. We plan to use NaNots first against FDA-recognized autoimmune and autoinflammatory diseases, then repurpose these NaNots to treat sepsis and inflammaging.
That’s on the inflammatory side. On the inhibitory side, we’re taking out four of the main inhibitory molecules that cancer uses to defend itself: soluble PD-L1, sTNF-R1, sTNF-R2, and soluble HLA-G. Some of these have been documented as active in senescent cells or in the general reduction of immune competence that comes with age. We want to treat FDA-recognized diseases, because these diseases are terrible, but also because therapeutics against FDA-recognized diseases can be prescribed off-label for longevity applications.
So, diseases like cancer are the gateway, but the idea is, instead of extinguishing fires, to find ways to treat the root cause eventually?
Yes, I’m totally down with that mission. I always have been.
What do you think of the current longevity field in general?
I think it’s poised to revolutionize medicine. Some of the breakthroughs that are happening in geroscience are going to spill over into how we understand and treat mainstream diseases as well. Longevity science has the potential to radically transform our lives, and the value creation is going to be phenomenal as well. People like Jim Mellon say that the anti-aging field is going to be the most valuable field in history. Investments in this space are going to pay dividends far beyond anything we’ve seen before. The time scale may be uncertain, but I think the basic premise is true.