Mitochondrial Damage May Drive Type 2 Diabetes
- It may cause insulin-producing beta cells to stop doing their jobs.
A new study suggests that damaged mitochondria activate the integrated stress response, which causes pancreatic β-cells, as well as liver and fat cells, to lose their identity and malfunction [1]. Blocking this response had benefits in mouse models.
The mitochondria-diabetes connection
Like with many diseases, the prevalence of type 2 diabetes grows with age. Therefore, age-related dysregulation of some kind contributes to the development of the disease. However, scientists have been struggling to unearth the exact causes.
The central feature of diabetes is the inability of β-cells that reside in the pancreas to produce insulin, which is needed to store glucose and maintain glucose homeostasis. To do their job, β-cells need energy, which comes from mitochondria. Mitochondrial dysfunction is a hallmark of aging, and since most cells have mitochondria, its impact on living organisms is wide and heterogeneous [2].
Mitochondrial dysfunction has long been linked to diabetes [3], but the causality direction remained unclear. Do failing mitochondria make beta cells worse at their job, or is it the other way around? In a new paper published in Science, researchers from the University of Michigan shed some light on this question, with potentially powerful implications for future therapies.
Cells from diabetic donors have bad mitochondria
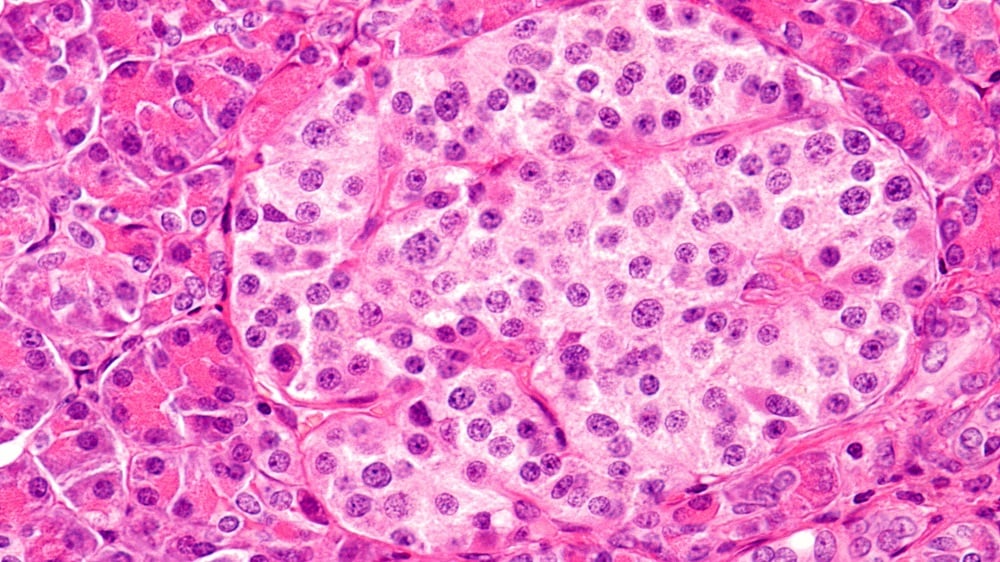
First, the scientists confirmed that human clusters of pancreatic endocrine cells (islets), including β-cells, from type 2 diabetes patients bear signs of mitochondrial dysfunction. Beta cells, but no other types of cells, from these patients had less mitochondrial DNA (mtDNA) and lower expression of 11 of 13 mitochondrial resident genes than in healthy controls. Mitophagy, the process of discarding malfunctioning mitochondria, was impaired as well.
These findings pointed at serious problems with the mechanisms of mitochondrial quality control. Interestingly, cells from simply obese donors or donors with insulin resistance did not show the same level of mitochondrial dysfunction, suggesting that this mitochondrial quality control loss was specific to diabetes patients.
How immature of you, β-cells
To see if impairing mitochondrial quality control can induce β-cell failure, the researchers engineered three mouse models with different mitochondrial pathways rendered deficient. The first model featured deletion of CLEC16A, a regulator of mitophagy, the second had reduced mtDNA content due to loss of TFAM, a regulator of mitochondrial genome integrity, and in the third, Mitofusins 1 and 2, proteins that promote mitochondrial fusion, were knocked out.
In all three models, messing with mitochondria triggered the integrated stress response (ISR). ISR is a cellular signaling network that is activated across various cell types to manage stress and maintain homeostasis by tweaking protein production. However, when persistently engaged, it can negatively impact cellular function. As they dug deeper to discover exactly how, the researchers received a surprise.
Apparently, mitochondria-to-nucleus (retrograde) ISR signaling dampened the expression of transcription factors that are central for β-cell maturity, identity, and function. As a result, the affected β-cells became less differentiated than their healthy counterparts.
“We wanted to determine which pathways are important for maintaining proper mitochondrial function,” said Dr. Emily M. Walker, a research assistant professor of internal medicine and first author of the study. “In all three cases, the exact same stress response was turned on, which caused β-cells to become immature, stop making enough insulin, and essentially stop being β-cells.”
Jamming the signal brings the cells back
Diabetes affects other metabolic tissues, such as liver tissue, muscle, and fat. To investigate further, the researchers ran similar experiments in mouse models of impaired mitochondrial quality control in liver cells (hepatocytes) and brown fat cells (adipocytes), with similar results.
“Diabetes is a multi-system disease: you gain weight, your liver produces too much sugar, and your muscles are affected. That’s why we wanted to look at other tissues as well,” said Scott A. Soleimanpour, M.D., director of the Michigan Diabetes Research Center and senior author of the study. “Although we haven’t tested all possible cell types, we believe that our results could be applicable to all the different tissues that are affected by diabetes.”
Can this be fixed? Several years ago, a potent ISR blocker called ISRIB was discovered and is currently in several clinical trials, including by Alphabet’s company Calico and the pharma giant AbbVie. The researchers treated mouse islets with ISRIB and found that it robustly restores β-cell identity markers specifically by inhibiting retrograde ISR signaling.
“Losing your β-cells is the most direct path to getting type 2 diabetes. Through our study we now have an explanation for what might be happening and how we can intervene and fix the root cause,” Soleimanpour said.
A possible basis for new treatments
Some other mitochondria researchers founded the study intriguing. “Using diet and genetic manipulations, the authors show the importance of robust mitophagy and retrograde signaling from mitochondria to nucleus in the involvement of mitochondrial function in type 2 diabetes,” said Dr. Amutha Boominathan, head of mitochondria research at the Longevity Research Institute. Boominathan and her team recently published an exciting study on nuclear expression of mitochondrial genes.
“What is interesting,” she added, “is that the authors find converging pathways in the β-Clec16aKO, β-Mfn1/2DKO and the Tfam-deficient mice in triggering the mitochondrial ISR influencing tissue specific blockade in cell differentiation not only in pancreas but also in other metabolic tissues such as liver and adipose tissues. The authors systematically address the causality for the role mitochondria play in age-associated metabolic diseases such as type 2 diabetes.”
Dr. Spring Behrouz, CEO of Vincere Biosciences, a mitochondria-targeting longevity biotech company, was impressed by the new study as well. “Reduced mtDNA levels, disrupted mitochondrial structure, and impaired mitophagy in metabolic tissues are often seen as secondary effects of other factors in type 2 diabetes,” she said. “However, this data suggests that early mitochondrial dysfunction actively contributes to the disease and potentially impacts other tissues.”
According to Behrouz, the study’s findings might be important for developing new mitochondria-based therapies. “By demonstrating the impact of mitochondrial quality control in metabolic tissue identity, this research opens up entirely new possibilities for treatment of diabetes as well as a range of other metabolic disorders,” she said.
Literature
[1] Walker, E. M., Pearson, G. L., Lawlor, N., Stendahl, A. M., Lietzke, A., Sidarala, V., … & Soleimanpour, S. A. (2025). Retrograde mitochondrial signaling governs the identity and maturity of metabolic tissues. Science, eadf2034.
[2] Srivastava, S. (2017). The mitochondrial basis of aging and age-related disorders. Genes, 8(12), 398.
[3] Kwak, S. H., Park, K. S., Lee, K. U., & Lee, H. K. (2010). Mitochondrial metabolism and diabetes. Journal of diabetes investigation, 1(5), 161-169.







