A Small Molecule Regenerates Cartilage in Aged Mice
- There are ramifications for long-term healing in younger people.

- 15-PGDH, which increases with age, harms tissue regeneration in animals.
- Inhibiting this molecule led to better outcomes in a murine model.
- Similar results were found in human cartilage in vitro.
By inhibiting the aging-related enzyme 15-PGDH, scientists have shifted cartilage cells towards a healthier phenotype, leading to a significant improvement in a mouse model of osteoarthritis [1].
The hard-to-repair part
Articular cartilage (the smooth, load-bearing cartilage on the ends of bones) doesn’t repair well with age or after injury [2], which is why osteoarthritis is hard to treat. This disease affects 1 in 5 adults, leading to reduced quality of life for 33 million patients in the US alone. Current treatments primarily focus on pain relief and joint replacement, with no approved therapies targeting the cartilage loss that causes osteoarthritis.
Previous research has shown that 15-hydroxyprostaglandin dehydrogenase (15-PGDH) increases with age in multiple tissues and can blunt regeneration by degrading key prostaglandins, lipid signaling molecules that influence inflammation and tissue repair. In those earlier models, which studied muscle, nerve, bone, and blood, inhibition of 15-PGDH boosted endogenous prostaglandin signaling and improved tissue repair [3].
Since osteoarthritis is fundamentally a problem of failed repair in articular cartilage, and cartilage regeneration strategies based on endogenous repair have been limited, a team led by researchers from Stanford Medicine decided to investigate the role of 15-PGDH in aged and injured cartilage. Their study was published in the journal Science.
More healthy cartilage
Using immunohistochemistry on knee joints from young (4 months) and aged (24 months) mice, the team discovered that cells expressing 15-PGDH were present in multiple joint tissues. In cartilage specifically, 15-PGDH abundance was about twice as high in aged mice. Aged knee joints had much thinner cartilage and multiple breaks in the cartilage surface.
A cohort of aged male mice was treated daily intraperitoneally with a small molecule 15-PGDH inhibitor (PGDHi) for one month. As a result, the knee joints of PGDHi-treated aged mice showed increased cartilage thickness and uniformness, almost on par with young mice.
The “extra” cartilage in treated aged mice was not fibrous and rough, as often happens after an injury heals, but bore many signs of normal cartilage, with increased expression of type II collagen (COL-2) and aggrecan (ACAN), the main structural building blocks of healthy cartilage, and of lubricin (PRG4), a surface lubricant that helps cartilage glide with low friction.
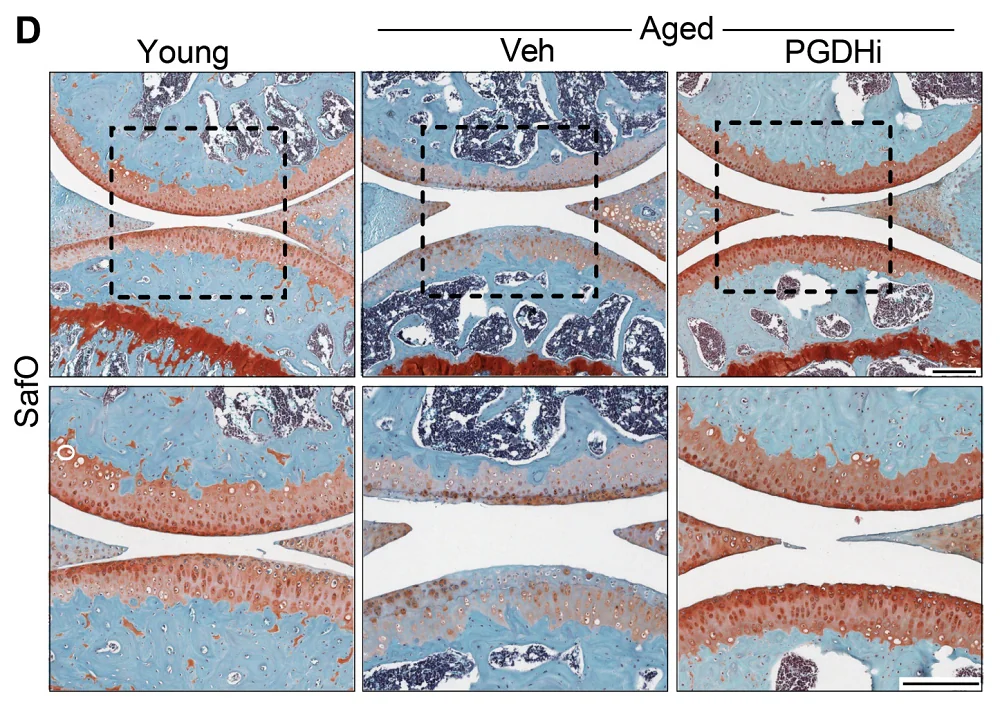
Safranin O staining: red/orange marks proteoglycan-rich cartilage matrix (healthier cartilage); fading indicates cartilage matrix depletion.
The researchers then wanted to know whether local joint delivery is sufficient in an injury-driven osteoarthritis model. Three-month-old male mice were treated with a series of intra-articular injections of PGDHi starting one week after injury, twice a week for two weeks.
The response was similar to what the team had seen with systemic administration: improved cartilage quality, higher COL-2, and increased aggrecan/lubricin. Pain responses were also better in treated mice: PGDHi-injected mice looked closer to uninjured controls across gait and mechanical pain measures. This particular experiment is relevant to young people as well: even after a successful repair, half of the people who suffer an ACL tear develop osteoarthritis in the injured joint within about 15 years.
No stem cells involved
Tissue regeneration often involves proliferation and differentiation of stem cells, but such cells in cartilage have rarely been seen, which might be a reason why cartilage regenerates poorly. The team made an exciting discovery: the regeneration they had witnessed was mostly due to gene expression changes in existing differentiated cartilage cells rather than a result of stem cell expansion.
The researchers identified multiple chondrocyte clusters in aged cartilage and described three that shift with PGDHi. Hypertrophic chondrocytes, the type that drives cartilage ossification, showed high expression of 15-PGDH. The treatment lowered the abundance of this subtype from 8% to 3%. Another largely harmful subset, fibro-chondrocytes, shifted from 16% down to 8% in the presence of PGDHi.
Conversely, the healthy subtype that actively maintains the extracellular matrix increased in prevalence from 22% to 42%. There was no evidence of drastically increased cellular division, supporting the idea that the positive effect mostly came from the existing cells shifting their behavior.
To make their findings more relevant to humans, the researchers studied samples from 11 osteoarthritis patients undergoing knee replacement and found signs of increased 15-PGDH expression and lower prostaglandin levels. Finally, they treated human cartilage with PGDHi in vitro and saw results similar to those in mice, with increased stiffness pointing to healthy load-bearing behavior.
“This is a new way of regenerating adult tissue, and it has significant clinical promise for treating arthritis due to aging or injury,” said Helen Blau, PhD, professor of microbiology and immunology and a senior author on the study. “We were looking for stem cells, but they are clearly not involved. We are very excited about this potential breakthrough. Imagine regrowing existing cartilage and avoiding joint replacement.”
“Millions of people suffer from joint pain and swelling as they age,” added Nidhi Bhutani, PhD, associate professor of orthopedic surgery, and another senior author. “It is a huge unmet medical need. Until now, there has been no drug that directly treats the cause of cartilage loss. But this [PGDH] inhibitor causes a dramatic regeneration of cartilage beyond that reported in response to any other drug or intervention. Cartilage regeneration to such an extent in aged mice took us by surprise. The effect was remarkable.”
Literature
[1] Singla, M., Wang, Y. X., Monti, E., Bedi, Y., Agarwal, P., Su, S., … & Bhutani, N. (2025). Inhibition of 15-hydroxy prostaglandin dehydrogenase promotes cartilage regeneration. Science, eadx6649.
[2] Hu H, et al. “Endogenous Repair and Regeneration of Injured Articular Cartilage: A Challenging Balance.” Cells. 2021.
[3] Palla, A. R., Ravichandran, M., Wang, Y. X., Alexandrova, L., Yang, A. V., Kraft, P., … & Blau, H. M. (2021). Inhibition of prostaglandin-degrading enzyme 15-PGDH rejuvenates aged muscle mass and strength. Science, 371(6528), eabc8059.