Study Uncovers How Obesity Drives Chronic Inflammation
- One particular pathway is crucial to the process.
- SAMHD1 prevents mitochondria from creating too much mitochondrial DNA, but this enzyme is inhibited in obese organisms.
- Too much mitochondrial DNA leads to an increase of the inflammatory factor NLRP3, which can lead to liver problems.
Scientists have discovered that obesity causes macrophages to ramp up mitochondrial DNA production, leading to more inflammation [1].
Obesity and inflammation
Obesity is associated with multiple acute and chronic conditions, including cardiovascular disease and various metabolic disorders [2]. Increased sterile (not pathogen-induced) chronic inflammation is a major mechanism behind this wide impact [3]. A new study from the University of Texas Southwestern Medical Center, published in Science, sheds light on one peculiar inflammatory pathway triggered by obesity.
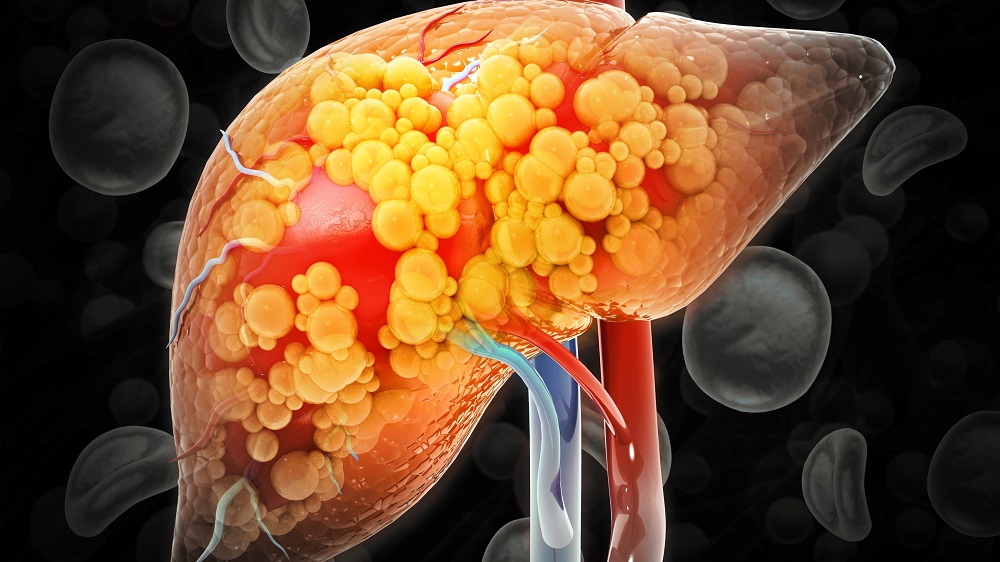
Obesity-associated sterile inflammation is largely driven by the activation of a protein complex called the NLRP3 inflammasome, primarily in macrophages. Activation of NLRP3 leads to the production of pro-inflammatory cytokines, especially IL-1β, which disrupts insulin signaling and promotes inflammation in the liver, contributing to conditions such as fatty liver (steatohepatitis), cirrhosis, and even cancer.
Why does NLRP3 get activated in the absence of pathogens? One mechanism involves mitochondrial DNA (mtDNA) sensing: when mitochondrial DNA leaks into the cytosol – especially in an oxidized form – it can act as a danger signal that strongly promotes NLRP3 activation.
mtDNA is subject to oxidative damage from reactive oxygen species (ROS). Oxidized mtDNA is a particularly strong NLRP3 trigger. More mtDNA also means more substrate that can become oxidized under mitochondrial stress.
Increased dNTP influx
The researchers wanted to know how obesity contributes to this dynamic. First, they took peripheral blood mononuclear cells (PBMCs) from lean and obese people and isolated monocytes, which were then differentiated into macrophages. Macrophages from obese individuals showed NLRP3 inflammasome hyperactivation and higher levels of mature IL-1β. Similar effects were observed in macrophages taken from mice on a high-fat diet.
Importantly, the levels of tumor necrosis factor (TNF), a central modulator of inflammation, were not elevated in cells derived from obese subjects, showing that the difference is in the specific NLRP3/IL-1β pathway rather than a broader inflammatory issue.
This hyperactivation correlated with elevated mtDNA levels in macrophages from obese subjects. These cells also produced more oxidized mtDNA following stimulation. Impeding mtDNA production or oxidized mtDNA binding to NLRP3 inhibited the obesity-linked NLRP3 hyperactivation.
Increased dNTP influx
MtDNA is produced from deoxyribonucleoside triphosphates (dNTPs). Mitochondria can obtain them via two main routes: the intramitochondrial salvage pathway and dNTPs from the cytosol. The researchers found that overproduction of mtDNA in obese subjects occurs mostly via the latter.
Since the enzyme SAMHD1 degrades excess dNTPs, preventing mitochondria from overproducing mtDNA, the researchers measured its expression and functional state. Apparently, cells from obese subjects have more phosphorylated SAMHD1, indicating inhibition of function. The researchers then prove that it’s specifically the loss of SAMHD1’s dNTP-degrading ability that causes the inflammation-related problems.
SAMHD1-deficient mice and zebrafish, as well as human macrophages, showed much higher IL-1β with NLRP3 triggers. The study reports that myeloid-specific SAMHD1 knockout mice on a high-fat diet developed insulin resistance and glucose intolerance compared with controls, despite similar body weight and composition. The animals also progressed towards steatohepatitis and fibrosis.
In their final mechanistic test, the authors asked whether excess dNTPs in the cytosol are actually feeding the inflammasome loop by being imported into mitochondria. They demonstrated that all four dNTPs accumulate when SAMHD1 is absent, consistent with the idea that mitochondria are being over-supplied. Pharmacologically blocking mitochondrial dNTP transport prevented the NLRP3 hyperactivation phenotype in SAMHD1-deficient mouse cells and in macrophages from obese human donors, supporting the idea that abnormal nucleotide influx helps drive mtDNA and oxidized mtDNA production that sensitizes NLRP3.
More energy – at a cost
In obesity, macrophages need lots of energy for jobs like phagocytosis and lysosomal cleanup. The authors suggest that SAMHD1 may be blunted to keep up with higher metabolic demands by increasing mitochondrial DNA synthesis. Instead of relying mainly on the slower, more energy-costly salvage pathway, macrophages may start importing ready-made dNTPs from the cytosol as a quicker alternative. The tradeoff is that this could also fuel NLRP3 hyperactivation, inflammation, and metabolic damage.
“It’s been known for a long time that obesity causes uncontrolled inflammation, but no one knew the mechanism behind it. Our study provides novel insights about why this inflammation occurs and how we might be able to stop it,” said Zhenyu Zhong, Ph.D., Assistant Professor of Immunology and member of the Harold C. Simmons Comprehensive Cancer Center at UT Southwestern, who co-led the study with Danhui Liu, Ph.D.
Literature
[1] Liu, D., Zhou, C., Wang, X., Luo, Z., Xu, R., Huo, S., … & Zhong, Z. (2026). Nucleotide metabolic rewiring enables NLRP3 inflammasome hyperactivation in obesity. Science, 391(6782), eadq9006.
[2] Powell-Wiley, T. M., Poirier, P., Burke, L. E., Després, J. P., Gordon-Larsen, P., Lavie, C. J., … & American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council. (2021). Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation, 143(21), e984-e1010.
[3] Rohm, T. V., Meier, D. T., Olefsky, J. M., & Donath, M. Y. (2022). Inflammation in obesity, diabetes, and related disorders. Immunity, 55(1), 31-55.