Building a Universal Immunotherapy for Cancer
- This improvement on previous techniques might quickly become a new standard of care.

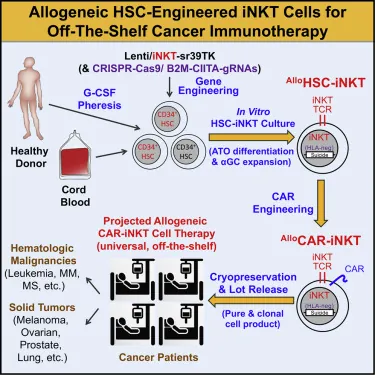
Researchers publishing in Cell Reports Medicine have described a method of using off-the-shelf, allogeneic immune cells as cancer therapy.
Overcoming the hurdles of allogeneic cells
Allogeneic cells come from other sources than the individual being treated. As recipients of organ donations know, if the immune system identifies foreign cells, it will attack them. This is known as graft-versus-host disease (GvHD), and it is why many organ recipients take immunosuppressants.
This problem is a major part of why the researchers chose to pursue an approach involving invariant natural killer T cells (iNKTs). They cite extensive prior research showing that these cells are excellent at attacking tumors through multiple methods while not inducing GvHD [1]. On paper, extracting and using iNKTs to fight cancer seems like a straightforward approach.
However, there are problems in extracting and using these cells. There are very few iNKT cells in blood [2], and extracting iNKT cells risks also extracting other immune cells that might cause GvHD. In order to sidestep this problem, the researchers had previously created cells in mice through genetic modification [3], although this approach is not sufficient for creating an off-the-shelf product.
To do that, they had to use a new, in vitro technique, which is the subject of this paper.
A multi-step approach with clear benefits
To develop this product, the researchers started with hemapoietic stem cells (HSCs) derived from human cord blood or peripheral blood stem cells (PBSCs). They used a lentiviral vector to encourage these cells to develop into iNKTs, then put them through a two-step process that stimulates their differentiation.
The researchers claim that half of the cells are successfully transfected by their vector and that the result is high in purity. One single donor of cord blood can result in 500 to 5,000 doses of the product, while a PBSC donor can provide anywhere from 30,000 to 300,000 doses, and the final product contains exceedingly few cells that would produce GvHD.
Through both direct examination and RNA sequence testing, these cells were shown to produce large amounts of cytokines and immune cell markers, which demonstrates their fitness for purpose. However, this wasn’t enough of a test; the researchers needed to test them against tumors themselves, in vitro and in mice.
In both cases, the cells performed well. When compared to PBMC-NK cells, which are taken from an endogenous source, these cells were much more effective in killing cancer cells and reducing the size of tumors. Interestingly, while those endogenous cells suffered significant damage from cryopreservation, the new HSC-iNKT cells did not.
HSC-iNKT cells were also found to be excellent at targeting specific types of cancers after chimeric antigen receptor (CAR) therapy:
The high antitumor efficacy and multiple tumor-targeting mechanisms of CAR-engineered AlloHSC-iNKT cells may provide new opportunities to target hard-to-treat tumors and counteract tumor antigen escape.
Conclusion
This paper outlines an entirely new method of generating T cells to fight cancer in a safe and consistently effective way. If the researchers’ clear optimism is shown to be warranted in human studies, allogeneic HSC-iNKT cells will quickly become the standard for cancer therapy, and cancer patients will expect oncologists to administer off-the-shelf immune therapies in much the same way as less advanced therapies are expected today.
Literature
[1] Fujii, S. I., Shimizu, K., Okamoto, Y., Kunii, N., Nakayama, T., Motohashi, S., & Taniguchi, M. (2013). NKT cells as an ideal anti-tumor immunotherapeutic. Frontiers in immunology, 4, 409.
[2] Krijgsman, D., Hokland, M., & Kuppen, P. J. (2018). The role of natural killer T cells in cancer—a phenotypical and functional approach. Frontiers in immunology, 9, 367.
[3] Zhu, Y., Smith, D. J., Zhou, Y., Li, Y. R., Yu, J., Lee, D., … & Yang, L. (2019). Development of hematopoietic stem cell-engineered invariant natural killer T cell therapy for cancer. Cell stem cell, 25(4), 542-557.







